Advanced Ultrasound in Diagnosis and Therapy ›› 2024, Vol. 8 ›› Issue (4): 195-204.doi: 10.37015/AUDT.2024.240058
• Review Articles • Previous Articles Next Articles
Li Zhenyia,1, Chen Yab,1, Wang Xinqic,d,1, Yang Lane, Chen Annib, Li Zhaojunb,d,*( ), Jin Lina,*(
), Jin Lina,*( )
)
Received:2024-10-08
Accepted:2024-12-26
Online:2024-12-30
Published:2024-11-12
Contact:
Li Zhaojun, Jin Lin,
E-mail:lzj_1975@sina.com;jinlin205@163.com
About author:First author contact:1 Zhenyi Li, Ya Chen, and Xinqi Wang contributed equally to this study.
Li Zhenyi, Chen Ya, Wang Xinqi, Yang Lan, Chen Anni, Li Zhaojun, Jin Lin. Left and Right Ventricular Interaction: Insight from Echocardiography Imaging. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 195-204.
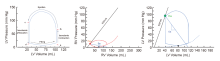
Figure 1
Pressure-Volume Loop of normal LV and RV. (A) The isovolumic contraction, ejection, isovolumic relaxation and ventricular filling phases of the cardiac cycle are shown in the LV pressure-volume plot. Point a, the point of maximum volume and minimum pressure corresponds to the end of diastole, the beginning of systole, and the closure of the mitral valve in the cycle. Point b, indicates that LVP rises above aortic pressure (AoP), at which point the aortic valve opens and begins to eject blood. Point c, the point at which LVP falls below AoP means the aortic valve closes and isovolumetric relaxation begins. Point d, LVP falls below LAP, the point at which the mitral valve opens and LV filling begins; (B) The RV loop exhibits a less prominent isovolumic period than the LV, and the top of the RV PV loop is more dome-shaped; (C) The LV ESPVR (Ees) (black line) has a much higher slope than the RV Ees. Ea (blue line), is coined the effective arterial elastance, that is, the elastance at the end of systole. Abbreviations: AoP, aortic pressure; Ea, arterial elastance; Ees, endsystolic elastance; ESPVR, endsystolic pressurevolume relationship; PV, pressure volume; LAP, left atrial pressure; LVP, left ventricular pressure; Pes, pressure at endsystole arterial elastance."
Table 1
Echocardiographic Parameters Reflecting Ventricular Interactions"
| Parameter | Author, year | Key findings |
|---|---|---|
| Septal shift | Burkett DA, et al. 2016 [ | Leftward septal shift directly interfering with LV filling (direct effect). Prolonged RV systole in PH, corresponding with leftward septal shift and impaired LV filling. |
| Interventricular septum motion | Banka VS, et al. 1981 [ | The IVS motion contributes equally to RV and LV function. |
| Ventricular septal motion | Welch TD, et al. 2014 [ | Shifting of the position of ventricular septum with inspiration is a manifestation of the phenomenon of interventricular dependence within a fixed space. |
| RV/LV ratio | Altmayer SPL, et al. 2018 [ | The RV/LV volume ratio of 2.3 or higher is associated with increased all-cause mortality in a PH population and should be considered as a cutoff for severe RV dilation. RV/LV ratio is an easily obtained, gender-independent, and a sensitive marker of RV dilation. |
| Ayöz S, et al. 2021 [ | RV/LV ratio should be evaluated together with cardiac biomarkers to define mortality risk. | |
| Jone PN, et al. 2014 [ | The RV/LV ratio incorporates both pathologic septal shift and RV dilation in children with PH and correlates with invasive measures of PH. An RV/LV ratio > 1 is associated with adverse clinical events. | |
| Eccentricity index | Ryan T, et al. 1985 [ | The eccentricity index is easily obtained, reproducible and can be applied to most patients with abnormal patterns of septal motion. |
| Burkett DA, et al. 2016 [ | Eccentricity index is related to LV echocardiographic diastolic measures. Weak negative correlations were seen between systolic eccentricity index with mitral E and E′/A′ and diastolic eccentricity index with mitral A′. | |
| LV eccentricity index (LVEI) | Koestenberger M, et al. 2019 [ | The LVEI can help guide clinicians as to whether relief of RV pressure overload is adequate. |
| Chiba Y, et al. 2022 [ | The early-diastolic LV eccentricity index reflects the degree of direct ventricular interaction owing to the RV pressure overload. | |
| RV to LV diameter ratio | Zhu L, et al. 2008 [ | The presence of RVD, the levels of RVED/LVED and SPAP were independent predictors of 14-day clinical outcomes. The predictive cut-off values of RVED/LVED and SPAP that yielded the highest discriminating power for adverse 14-day outcomes were 0.67 and 60 mm Hg, respectively. |
| Katterle KR, et al. 2023 [ | Existing risk stratification methods for acute PE, including RV/LV diameter ratio and BNP, are not accurate in patients with a history of HF, especially HFrEF | |
| Systolic-diastolic duraton ratio | Alkon J, et al. 2010 [ | A high S:D ratio is associated with worse RV function and hemodynamics and worse functional capacity. |
| McCrary AW, et al. 2016 [ | With either SD dysfunction the duration of systole increases and diastole decreases, producing an elevated SD ratio > 1. Multiple alterations in cardiac structure and function contribute to an elevated SD ratio. | |
| Early diastolic biphasic septal motion and polyphasic fluttering | Sengupta PP, et al. 2005 [ | The ventricular septum moves abruptly to the LV on inhalation and in the opposite direction on exhalation, reflecting an exaggerated interventricular interdependence and abnormal early and late diastolic notching. |
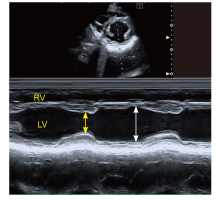
Figure 3
Echocardiographic Parasternal M-Mode Depicting Transverse RV Shortening Fraction as a Measure of RV Dysfunction. End-diastolic dimension is depicted by the yellow arrow and end-systolic dimension by the white arrow. LV and RV contraction are highly aligned and septal position is neutral. LV, left ventricular; RV, right ventricular."
| [1] | Brener MI, Kanwar MK, Lander MM, Hamid NB, Raina A, Sethi SS, et al. Impact of interventricular interaction on ventricular function: Insights from right ventricular pressure-volume analysis. JACC Heart Fail 2024; 12:1179-1192. |
| [2] |
Friedberg MK. Imaging right-left ventricular interactions. JACC Cardiovasc Imaging 2018; 11:755-771.
doi: S1936-878X(18)30200-6 pmid: 29747850 |
| [3] |
Santamore WP, Dell'Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis 1998; 40:289-308.
doi: 10.1016/s0033-0620(98)80049-2 pmid: 9449956 |
| [4] | D B. De l’asystolie veineuse dans l’hypertrophie du cœur gauche par ste ́nose concomitante du ventricule droit. J Rev Med 1910; 39:785-801. |
| [5] | Y H, AL P. The relative systolic discharges of the right and left ventricles and their bearing on pulmmonary congestion and depletion. J Heart 1914; 5: 217-226. |
| [6] | DEXTER L. Atrial septal defect. J Br Heart J 1956; 18:209-225. |
| [7] | Kroeker CA, Shrive NG, Belenkie I, Tyberg JV. Pericardium modulates left and right ventricular stroke volumes to compensate for sudden changes in atrial volume. Am J Physiol Heart Circ Physiol 2003; 284:H2247-2254. |
| [8] | Robotham JL, Mintzner W. A model of the effects of respiration on left ventricular performance. J Appl Physiol Respir Environ Exerc Physiol 1979; 46:411-418. |
| [9] |
Fan L, Choy JS, Lee S, Campbell KS, Wenk JF, Kassab GS, et al. An in silico study of the effects of left ventricular assist device on right ventricular function and inter-ventricular interaction. Artif Organs 2023; 47:1831-1847.
doi: 10.1111/aor.14649 pmid: 37746896 |
| [10] |
Yamaguchi S, Harasawa H, Li KS, Zhu D, Santamore WP. Comparative significance in systolic ventricular interaction. Cardiovasc Res 1991; 25:774-783.
pmid: 1799909 |
| [11] | Damiano RJ Jr, La Follette P Jr, Cox JL, Lowe JE, Santamore WP. Significant left ventricular contribution to right ventricular systolic function. Am J Physiol 1991; 261:H1514-1524. |
| [12] | Slinker BK, Chagas AC, Glantz SA. Chronic pressure overload hypertrophy decreases direct ventricular interaction. Am J Physiol 1987; 253:H347-357. |
| [13] |
Farrar DJ, Chow E, Brown CD. Isolated systolic and diastolic ventricular interactions in pacing-induced dilated cardiomyopathy and effects of volume loading and pericardium. Circulation 1995; 92:1284-1290.
pmid: 7648677 |
| [14] | Hoffman D, Sisto D, Frater RW, Nikolic SD. Left-to-right ventricular interaction with a noncontracting right ventricle. J Thorac Cardiovasc Surg 1994; 107:1496-1502. |
| [15] | Pinsky MR. Dynamic right and left ventricular interactions in the pig. Exp Physiol 2020; 105:1293-1315. |
| [16] | Amsallem M, Mercier O, Kobayashi Y, Moneghetti K, Haddad F. Forgotten no more: A focused update on the right ventricle in cardiovascular disease. JACC Heart Fail 2018; 6:891-903. |
| [17] |
Weber KT, Janicki JS, Shroff S, Fishman AP. Contractile mechanics and interaction of the right and left ventricles. Am J Cardiol 1981; 47:686-695.
pmid: 7008570 |
| [18] |
Hoit BD. Anatomy and physiology of the pericardium. Cardiol Clin 2017; 35:481-490.
doi: S0733-8651(17)30062-0 pmid: 29025540 |
| [19] | Fritz T, Wieners C, Seemann G, Steen H, Dössel O. Simulation of the contraction of the ventricles in a human heart model including atria and pericardium. Biomech Model Mechanobiol 2014; 13:627-641. |
| [20] |
Spadaro J, Bing OH, Gaasch WH, Weintraub RM. Pericardial modulation of right and left ventriclar diastolic interaction. Circ Res 1981; 48:233-238.
pmid: 7460199 |
| [21] |
Schertz C, Pinsky MR. Effect of the pericardium on systolic ventricular interdependence in the dog. J Crit Care 1993; 8:17-23.
pmid: 8343855 |
| [22] |
Maughan WL, Kallman CH, Shoukas A. The effect of right ventricular filling on the pressure-volume relationship of ejecting canine left ventricle. Circ Res 1981; 49:382-388.
pmid: 7249274 |
| [23] | Bouchez S, Erb J, Foubert L, Mauermann E. Pressure-volume loops for reviewing right ventricular physiology and failure in the context of left ventricular assist device implantation. Semin Cardiothorac Vasc Anesth 2023; 27:283-291. |
| [24] | Brener MI, Masoumi A, Ng VG, Tello K, Bastos MB, Cornwell WK 3rd, et al. Invasive right ventricular pressure-volume analysis: basic principles, clinical applications, and practical recommendations. Circ Heart Fail 2022; 15:e009101. |
| [25] | Faber MJ, Dalinghaus M, Lankhuizen IM, Steendijk P, Hop WC, Schoemaker RG, et al. Right and left ventricular function after chronic pulmonary artery banding in rats assessed with biventricular pressure-volume loops. Am J Physiol Heart Circ Physiol 2006; 291:H1580-1586. |
| [26] | Li VW, Yu CK, So EK, Wong WH, Cheung YF. Ventricular myocardial deformation imaging of patients with repaired tetralogy of fallot. J Am Soc Echocardiogr 2020; 33:788-801. |
| [27] | Lammers AE, Haworth SG, Riley G, Maslin K, Diller GP, Marek J. Value of tissue Doppler echocardiography in children with pulmonary hypertension. J Am Soc Echocardiogr 2012; 25:504-510. |
| [28] |
Popp RL, Wolfe SB, Hirata T, Feigenbaum H. Estimation of right and left ventricular size by ultrasound. A study of the echoes from the interventricular septum. Am J Cardiol 1969; 24:523-530.
pmid: 5811535 |
| [29] | Burkett DA, Slorach C, Patel SS, Redington AN, Ivy DD, Mertens L, et al. Left ventricular myocardial function in children with pulmonary hypertension: relation to right ventricular performance and hemodynamics. Circ Cardiovasc Imaging 2015; 8:10.1161 |
| [30] | Koestenberger M, Sallmon H, Avian A, Cantinotti M, Gamillscheg A, Kurath-Koller S, et al. Ventricular-ventricular interaction variables correlate with surrogate variables of clinical outcome in children with pulmonary hypertension. Pulm Circ 2019; 9:2045894019854074. |
| [31] | Lammers AE, Apitz C, Michel-Behnke I, Koestenberger M. A guide to echocardiographic assessment in children and adolescents with pulmonary hypertension. Cardiovasc Diagn Ther 2021; 11:1160-1177. |
| [32] |
Ghio S, Klersy C, Magrini G, D'Armini AM, Scelsi L, Raineri C, et al. Prognostic relevance of the echocardiographic assessment of right ventricular function in patients with idiopathic pulmonary arterial hypertension. Int J Cardiol 2010; 140:272-278.
doi: 10.1016/j.ijcard.2008.11.051 pmid: 19070379 |
| [33] | Koestenberger M, Hansmann G. Left ventricular geometry and near-simultaneous invasive hemodynamics in pediatric pulmonary hypertension. Circ Cardiovasc Imaging 2020; 13:e010787. |
| [34] | Koestenberger M, Friedberg MK, Ravekes W, Nestaas E, Hansmann G. Non-invasive imaging for congenital heart disease: recent innovations in transthoracic echocardiography. J Clin Exp Cardiolog 2012; Suppl 8:2. |
| [35] |
Driessen MMP, Meijboom FJ, Hui W, Dragulescu A, Mertens L, Friedberg MK. Regional right ventricular remodeling and function in children with idiopathic pulmonary arterial hypertension vs those with pulmonary valve stenosis: Insights into mechanics of right ventricular dysfunction. Echocardiography 2017; 34:888-897.
doi: 10.1111/echo.13529 pmid: 28370259 |
| [36] |
Nestaas E, Schubert U, de Boode WP, El-Khuffash A; European Special Interest Group ‘Neonatologist Performed Echocardiography’ NPE. Tissue Doppler velocity imaging and event timings in neonates: a guide to image acquisition, measurement, interpretation, and reference values. Pediatr Res 2018; 84:18-29.
doi: 10.1038/s41390-018-0079-8 pmid: 30072806 |
| [37] | Rowland T, Heffernan K, Jae SY, Echols G, Fernhall B. Tissue Doppler assessment of ventricular function during cycling in 7- to 12-yr-old boys. Med Sci Sports Exerc 2006; 38:1216-1222. |
| [38] | Ahmad N, Kantor PF, Grosse-Wortmann L, Seller N, Jaeggi ET, Friedberg MK, Mertens L. Influence of RV restrictive physiology on LV diastolic function in children after tetralogy of Fallot repair. J Am Soc Echocardiogr 2012; 25:866-873. |
| [39] |
Chow PC, Liang XC, Cheung EW, Lam WW, Cheung YF. New two-dimensional global longitudinal strain and strain rate imaging for assessment of systemic right ventricular function. Heart 2008; 94:855-859.
doi: 10.1136/hrt.2007.131862 pmid: 18230639 |
| [40] | Li SJ, Yu HK, Wong SJ, Cheung YF. Right and left ventricular mechanics and interaction late after balloon valvoplasty for pulmonary stenosis. Eur Heart J Cardiovasc Imaging 2014; 15:1020-1028. |
| [41] | Bharucha T, Viola N. The tricuspid valve in hypoplastic left heart syndrome: Echocardiography provides insight into anatomy and function. Front Pediatr 2023; 11:1145161. |
| [42] |
Simpson J, Lopez L, Acar P, Friedberg M, Khoo N, Ko H, et al. Three-dimensional echocardiography in congenital heart disease: an expert consensus document from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging 2016; 17:1071-1097.
doi: 10.1093/ehjci/jew172 pmid: 27655864 |
| [43] | Nagata Y, Wu VC, Kado Y, Otani K, Lin FC, Otsuji Y, et al. Prognostic value of right ventricular ejection fraction assessed by transthoracic 3D echocardiography. Circ Cardiovasc Imaging 2017; 10:e005384. |
| [44] | Ghio S, Acquaro M, Agostoni P, Ambrosio G, Carluccio E, Castiglione V, et al. Right heart failure in left heart disease: imaging, functional, and biochemical aspects of right ventricular dysfunction. Heart Fail Rev 2023; 28:1009-1022. |
| [45] |
Yamamuro M, Tadamura E, Kubo S, Toyoda H, Nishina T, Ohba M, et al. Cardiac functional analysis with multi-detector row CT and segmental reconstruction algorithm: comparison with echocardiography, SPECT, and MR imaging. Radiology. 2005; 234:381-390.
pmid: 15670995 |
| [46] | Claessen G, Claus P, Delcroix M, Bogaert J, La Gerche A, Heidbuchel H. Interaction between respiration and right versus left ventricular volumes at rest and during exercise: a real-time cardiac magnetic resonance study. Am J Physiol Heart Circ Physiol 2014; 306:H816-824. |
| [47] | Asferg C, Usinger L, Kristensen TS, Abdulla J. Accuracy of multi-slice computed tomography for measurement of left ventricular ejection fraction compared with cardiac magnetic resonance imaging and two-dimensional transthoracic echocardiography: a systematic review and meta-analysis. Eur J Radiol 2012; 81:e757-762. |
| [48] | Sayyed SH, Cassidy MM, Hadi MA. Use of multidetector computed tomography for evaluation of global and regional left ventricular function. J Cardiovasc Comput Tomogr 2009; 3:S23-34. |
| [49] |
Schmitt B, Fedarava K, Falkenberg J, Rothaus K, Bodhey NK, Reischauer C, et al. Three-dimensional alignment of the aggregated myocytes in the normal and hypertrophic murine heart. J Appl Physiol (1985) 2009; 107:921-927.
doi: 10.1152/japplphysiol.00275.2009 pmid: 19628727 |
| [50] | Nielsen E, Smerup M, Agger P, Frandsen J, Ringgard S, Pedersen M, et al. Normal right ventricular three-dimensional architecture, as assessed with diffusion tensor magnetic resonance imaging, is preserved during experimentally induced right ventricular hypertrophy. Anat Rec (Hoboken) 2009; 292:640-651. |
| [51] |
Hoffman JI. Abraham Morris Rudolph: an appreciation. Pediatrics 2002; 110:622-626.
pmid: 12205269 |
| [52] |
Naeije R, Badagliacca R. The overloaded right heart and ventricular interdependence. Cardiovasc Res 2017; 113:1474-1485.
doi: 10.1093/cvr/cvx160 pmid: 28957537 |
| [53] |
Strong C, Raposo L, Castro M, Madeira S, Tralhão A, Ventosa A, et al. Haemodynamic effects and potential clinical implications of inhaled nitric oxide during right heart catheterization in heart transplant candidates. ESC Heart Fail 2020; 7:673-681.
doi: 10.1002/ehf2.12639 pmid: 32045139 |
| [54] |
Rother RP, Bell L, Hillmen P, Gladwin MT. The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: a novel mechanism of human disease. JAMA 2005; 293:1653-1662.
doi: 10.1001/jama.293.13.1653 pmid: 15811985 |
| [55] |
Van Tosh A, Nichols KJ. Ventricular asynchrony: A shift to the right? J Nucl Cardiol 2017; 24:79-82.
doi: 10.1007/s12350-015-0383-1 pmid: 26747435 |
| [56] |
Kyriakides ZS, Manolis AG, Kolettis TM. The effects of ventricular asynchrony on myocardial perfusion. Int J Cardiol 2007; 119:3-9.
pmid: 17056140 |
| [57] |
Santamore WP, Li KS, Nakamoto T, Johnston WE. Effects of increased pericardial pressure on the coupling between the ventricles. Cardiovasc Res 1990; 24:768-776.
pmid: 2224943 |
| [58] |
Comunale G, Peruzzo P, Castaldi B, Razzolini R, Di Salvo G, Padalino MA, Susin FM. Understanding and recognition of the right ventricular function and dysfunction via a numerical study. Sci Rep 2021; 11:3709.
doi: 10.1038/s41598-021-82567-9 pmid: 33580128 |
| [59] |
Lumens J, Ploux S, Strik M, Gorcsan J 3rd, Cochet H, Derval N, et al. Comparative electromechanical and hemodynamic effects of left ventricular and biventricular pacing in dyssynchronous heart failure: electrical resynchronization versus left-right ventricular interaction. J Am Coll Cardiol 2013; 62:2395-2403.
doi: S0735-1097(13)04002-3 pmid: 24013057 |
| [60] | Friedberg MK, Wu S, Slorach C. Left-right ventricular interactions in pediatric aortic stenosis: right ventricular myocardial strain before and after aortic valvuloplasty. J Am Soc Echocardiogr 2013; 26:390-397. |
| [61] | Graham T P. Ventricular performance in congenital heart disease. J Circulation 1991; 84:2259-2274. |
| [62] | Yang EL, Kutty S, Soriano BD, Mallenahalli S, Ferguson MR, Lewin MB, Buddhe S. Is biventricular vascular coupling a better indicator of ventriculo-ventricular interaction in congenital heart disease? Cardiol Young 2021; 31:2009-2014. |
| [63] | Burkett DA, Slorach C, Patel SS, Redington AN, Ivy DD, Mertens L, et al. Impact of pulmonary hemodynamics and ventricular interdependence on left ventricular diastolic function in children with pulmonary hypertension. Circ Cardiovasc Imaging 2016; 9:10.1161/CIRCIMAGING.116.004612 e004612. |
| [64] |
Banka VS, Agarwal JB, Bodenheimer MM, Helfant RH. Interventricular septal motion: biventricular angiographic assessment of its relative contribution to left and right ventricular contraction. Circulation 1981; 64:992-996.
pmid: 7285313 |
| [65] |
Welch TD, Ling LH, Espinosa RE, Anavekar NS, Wiste HJ, Lahr BD, et al. Echocardiographic diagnosis of constrictive pericarditis: Mayo Clinic criteria. Circ Cardiovasc Imaging 2014; 7:526-534.
doi: 10.1161/CIRCIMAGING.113.001613 pmid: 24633783 |
| [66] |
Altmayer SPL, Han QJ, Addetia K, Patel AR, Forfia PR, Han Y. Using all-cause mortality to define severe RV dilation with RV/LV volume ratio. Sci Rep 2018; 8:7200.
doi: 10.1038/s41598-018-25259-1 pmid: 29739967 |
| [67] | Ayöz S, Erol S, Kul M, Gürün Kaya A, Gürsoy Çoruh A, Savaş İ, et al. Using RV/LV ratio and cardiac biomarkers to define the risk of mortality from pulmonary embolism. Tuberk Toraks 2021; 69:297-306. |
| [68] | Jone PN, Hinzman J, Wagner BD, Ivy DD, Younoszai A. Right ventricular to left ventricular diameter ratio at end-systole in evaluating outcomes in children with pulmonary hypertension. J Am Soc Echocardiogr 2014; 27:172-178. |
| [69] |
Ryan T, Petrovic O, Dillon JC, Feigenbaum H, Conley MJ, Armstrong WF. An echocardiographic index for separation of right ventricular volume and pressure overload. J Am Coll Cardiol 1985; 5:918-927.
doi: 10.1016/s0735-1097(85)80433-2 pmid: 3973294 |
| [70] | Chiba Y, Iwano H, Tsuneta S, Tsujinaga S, Meyers B, Vlachos P, et al. Determinants of altered left ventricular suction in pre-capillary pulmonary hypertension. Eur Heart J Cardiovasc Imaging 2022; 23:1399-1406. |
| [71] |
Zhu L, Yang Y, Wu Y, Zhai Z, Wang C. Value of right ventricular dysfunction for prognosis in pulmonary embolism. Int J Cardiol 2008; 127:40-45.
pmid: 17716753 |
| [72] |
Katterle KR, Niedoba MJ, Pasadyn VE, Mann A, Brewster PS, Dasa O, et al. Impact of baseline heart failure on acute pulmonary embolism risk stratification and clinical outcomes. Am J Cardiol 2023; 200:26-31.
doi: 10.1016/j.amjcard.2023.05.008 pmid: 37276720 |
| [73] |
Alkon J, Humpl T, Manlhiot C, McCrindle BW, Reyes JT, Friedberg MK. Usefulness of the right ventricular systolic to diastolic duration ratio to predict functional capacity and survival in children with pulmonary arterial hypertension. Am J Cardiol 2010; 106:430-436.
doi: 10.1016/j.amjcard.2010.03.048 pmid: 20643259 |
| [74] |
McCrary AW, Malowitz JR, Hornick CP, Hill KD, Cotten CM, Tatum GH, Barker PC. Differences in eccentricity index and systolic-diastolic ratio in extremely low-birth-weight infants with bronchopulmonary dysplasia at risk of pulmonary hypertension. Am J Perinatol 2016; 33:57-62.
doi: 10.1055/s-0035-1556757 pmid: 26171597 |
| [75] | Sengupta PP, Mohan JC, Mehta V, Arora R, Khandheria BK, Pandian NG. Doppler tissue imaging improves assessment of abnormal interventricular septal and posterior wall motion in constrictive pericarditis. J Am Soc Echocardiogr 2005; 18:226-230. |
| [1] | Zhang Xin, Yang Yun, Zhang Ruize, Zhang Linyue, Xie Yuji, Wu Wenqian, Zhang Jing, Lv Qing, Wang Jing, Xie Mingxing. Noninvasive Evaluation of Left Ventricular-Arterial Coupling: Methodologies and Clinical Relevance [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 149-158. |
| [2] | Chen Anni, Yang Lan, Li Zhenyi, Wang Xinqi, Chen Ya, Jin Lin, Li Zhaojun. Left Ventricular-Arterial Coupling in Cardiovascular Health: Development, Assessment Methods, and Future Directions [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 159-171. |
| [3] | Yang Yun, Zhang Xin, Zhang Ruize, Jiang Jingrong, Xie Yuji, Fang Lingyun, Zhang Jing, Xie Mingxing, Wang Jing. Current Status and Progress in Arterial Stiffness Evaluation: A Comprehensive Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 172-182. |
| [4] | Chen Ya, Wang Xinqi, Chen Anni, Li Zhenyi, Yang Lan, Li Zhaojun, Jin Lin, Wang Xifu. The Application and Research Progress of Cardiac Magnetic Resonance in the Assessment of Right Ventricular-Pulmonary Arterial Coupling [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 183-194. |
| [5] | Wang Xinqi, Chen Anni, Yang Lan, Chen Ya, Li Zhenyi, Li Zhaojun, Jin Lin. Evaluation Methods and Progress of Right Ventricular-pulmonary Artery Coupling [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 205-216. |
| [6] | Junrong Hong, MD, Pingyang Zhang, MD, PhD, Mengyao Fei, MD, Lingling Wang, MD. A Study on Left Atrial Function in Patients with Essential Hypertension Using Four-Dimensional Echocardiography [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(2): 64-73. |
| [7] | Guiwu Chen, MS, Zhizhong He, BS, Wenqin Liu, MS, Junjun Chen, BS, Xiaomin Liao, MS, Yuhuan Xie, BS. Multimodal Sonographic Findings of Embryonal Carcinoma in the Testis: A Case Report and Literature Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(2): 74-77. |
| [8] | Guoying Zhang, MD, Ying Tang, BS, Mingyang Wang, MD, Weina Kong, MD. Diagnostic Utility of Superb Microvascular Imaging of ultrasound Examinations to Evaluate Hepatic Ischemia-reperfusion Injury [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(1): 15-21. |
| [9] | Cong Wei, MD, Hui Zhang, PhD, Tao Ying, MD, Bing Hu, MD, Yini Chen, MD, Hongtao Li, MD, Qiude Zhang, PhD, Mingyue Ding, PhD, Jie Chen, MD, Ming Yuchi, PhD, Yuanyi Zheng, MD. Clinical Application of Ultrasound Tomography in Diagnosis of Musculoskeletal Diseases [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(1): 7-14. |
| [10] | Yang Qi, MD, Dengsheng Sun, MD, Linyao Wang, MD, Jie Yu, MD, Ping Liang, MD. State-of-the-Art and Development Trend of Interventional Ultrasound in China [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(4): 313-320. |
| [11] | Osama Mahmoud, BS, Ajay Makkena, BS, Corinne E. Wessner, MS, MBA, RDMS, Ji-Bin Liu, MD, John R. Eisenbrey, PhD, Andrej Lyshchik, MD, PhD. Contrast-Enhanced Ultrasound LI-RADS: A Pictorial Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(4): 321-332. |
| [12] | Wenwen Chen, BS, Yuji Xie, MD, Zisang Zhang, MD, Ye Zhu, MS, Yiwei Zhang, MD, Shuangshuang Zhu, MD, PhD, Chun Wu, MD, PhD, Ziming Zhang, MD, Xin Yang, PhD, Man wei Liu, MD, PhD, Mingxing Xie, MD, PhD, Li Zhang, MD, PhD. Artificial Intelligence-assisted Medical Imaging in Interventional Management of Valvular Heart Disease [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(3): 217-227. |
| [13] | Bo Jiang, MD, Yiman Du, MD, Xiang Fei, MD, Jianing Zhu, MD, Lianhua Zhu, MD, Qiuyang Li, MD, Yukun Luo, MD, PhD. Ultrasound-Guided Attenuation Parameter May Replace B-mode Ultrasound in Diagnosing Nonalcoholic Fatty Liver Disease [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(3): 260-266. |
| [14] | Xiuping Men, PhD, Vladimir Y. Mariano, PhD, Aihua Duan, PhD, Xiaoyan Shi, PhD. Lung Nodule Classification in CT Images Using Improved DenseNet [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(3): 272-278. |
| [15] | Tianxiang Li, BS, Fei Ji, BS, Ruina Zhao, MD, Huazhen Liu, MD, Meng Yang, MD. Advances in the Research of Ultrasound and Artificial Intelligence in Neuromuscular Disease [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(2): 122-129. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
Share: WeChat
Copyright ©2018 Advanced Ultrasound in Diagnosis and Therapy
|
 Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
