Advanced Ultrasound in Diagnosis and Therapy ›› 2024, Vol. 8 ›› Issue (4): 159-171.doi: 10.37015/AUDT.2024.240057
• Review Articles • Previous Articles Next Articles
Chen Annia,b,1, Yang Lanc,1, Li Zhenyid,1, Wang Xinqie, Chen Yaa, Jin Lind,*( ), Li Zhaojuna,b,*(
), Li Zhaojuna,b,*( )
)
Received:2024-10-07
Accepted:2024-12-24
Online:2024-12-30
Published:2024-11-12
Contact:
Jin Lin, Li Zhaojun,
E-mail:jinlin205@163.com;lzj_1975@sina.com
About author:First author contact:1Anni Chen, Lan Yang, and Zhenyi Li contributed equally to this study.
Chen Anni, Yang Lan, Li Zhenyi, Wang Xinqi, Chen Ya, Jin Lin, Li Zhaojun. Left Ventricular-Arterial Coupling in Cardiovascular Health: Development, Assessment Methods, and Future Directions. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 159-171.
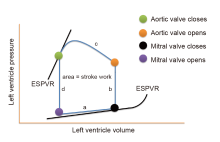
Figure 1
Left ventricular pressure-volume loop representing the relationship between intraventricular pressure (ordinate) and volume (abscissa) during a single cardiac cycle. (a, filling; b, isovolumetric contraction, IVC; c, ejection; d, isovolumetric relaxation, IVR). Area, stroke volume; ESPVR, end-systolic pressure-volume ratio; EDPVR, end-dystolic pressure-volume ratio."
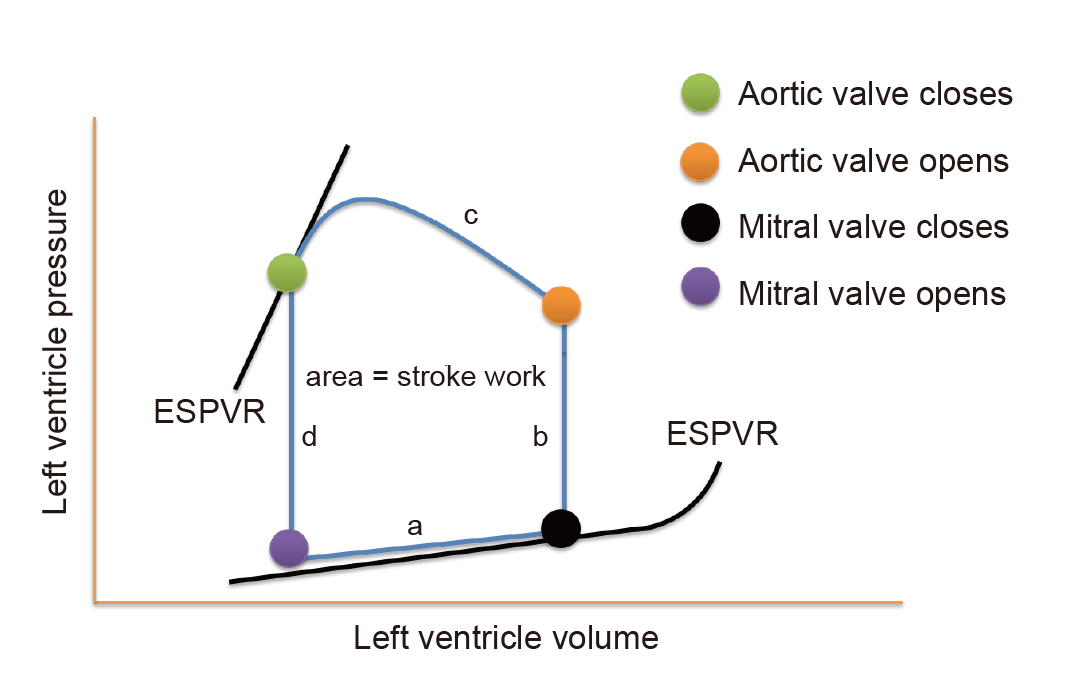
Table 1
Key stages in the history of left ventricular-arterial coupling research and development"
| Year | Author | Research finds |
|---|---|---|
| 1920s | Otto Frank Ernest Starling [ | Established the theoretical foundation for the interaction between cardiac function and vascular system, known as the "Frank-Starling law", which elucidates the relationship between cardiac output and arterial compliance. |
| 1974 | Suga Sagawa [ | Introduced the pressure-volume relationship model, which characterizes the alignment between LV contractility and the arterial system. |
| 1981 | Sagawa [ | The concept of ESPVR, one of the core metrics for studying LVAC, was proposed. |
| 1983 | Sunagawa [ | VAC was further developed, and Ea and Ees were proposed for evaluating the coupling of the LV and arterial systems. |
| 1980s (1983) | Sunagawa with his colleagues [ | VAC was further investigated and subdivided into LVAC and RVAC, a phase of research that greatly advanced the understanding of the pathophysiologic mechanisms of cardiovascular diseases (such as HF, hypertension). |
| 1992 | Kelly Ting [ | Explored Ea as a marker of arterial load, marking the initial clinical application of the LVAC concept. |
| 2013 | Chirinos [ | LVAC is widely used to assess pathologies such as HF, CAD, and hypertension. Therapeutic strategies to help clinicians optimize cardiac function. |
Table 2
Advantages and disadvantages of left ventricular-arterial coupling assessment methods"
| Assessment modality | Advantages | Disadvantages |
|---|---|---|
| Cardiac catheterization [ | Direct measurement of pressure and volume enables accurate assessment of coupling conditions Real-time assessment of LV function and arterial load The gold standard for assessing Ees and Ea | Highly invasive, with risks including infection, bleeding, and other complications Costly |
| Pressure-volume loop [ | Accurate assessment of cardiac function Assess changes in the heart under different loading conditions | Highly invasive and may cause complications Technically complex and costly |
| PWA [ | A non-invasive examination with low risk Ease of operation, suitable for large-scale population screening and follow-up | Direct assessment of LV function is more limited Results are more influenced by the measurement site and technical maneuvers May not be as accurate as invasive methods |
| Echocardiography [ | Non-invasive, convenient, and inexpensive Suitable for assessing LV function in a variety of clinical settings Provide additional information on cardiac structure and function (such as EF and myocardial strain rate). | Highly influenced by operator skill level and imaging conditions Indirect estimation of Ees and Ea may be subject to some error |
| CMR [ | Non-invasive imaging techniques Accurate measurement of the three-dimensional structure and function of the heart Very high imaging resolution High precision and reliability | Higher costs Long inspection time Restrictive to patients (such as cannot be used in patients with metal implants) |
| AI, ML [ | Saves data processing time, improves the efficiency of assessments Enable greater accuracy and consistency in complex clinical environments Provide personalized LVAC prediction and treatment recommendations | Based on computer models, not yet validated in clinical models Requires very advanced and expensive computer equipment |
Table 3
Advantages and disadvantages of left ventricular-arterial coupling evaluation metrics"
| Evaluation metrics | Advantages | Disadvantages |
|---|---|---|
| Ventricular afterload | ||
| Ea | A key indicator of ventricular afterload Accurately reflecting the compliance and resistance of the arterial system | Usually requires invasive or semi-invasive measurements and is not applicable to all patients, especially in acute situations Susceptible to significant influences of heart rate and is not a pure index of arterial load Complex to calculate Depends mainly on resistance and is not sensitive to changes in pulsatile arterial load |
| Aortic impedance | Reflects the dynamic interaction between the heart and the arterial system, and is an accurate assessment of ventricular afterload Closely related to the compliance, elasticity, and other characteristics of the cardiovascular system, and can be used to assess atherosclerosis and other pathologies | Complex to measure, often requiring invasive or sophisticated measurement tools such as pressure catheters and ultrasonic devices More sensitive to hydrodynamic conditions and may be affected by changes in heart rate and hemodynamics |
| SVR | Assesses the total resistance of blood vessels to pumping by the heart and is suitable for assessing overall hemodynamic Easy to calculate, commonly measured by hemodynamic monitoring tools, and quick to use in acute situations | Only reflects overall resistance, not arterial elasticity or microvascular resistance accurately Insensitive to small vessel disease or local arterial stiffness |
| Arterial blood pressure (especially MAP ) | Widely used, simple and without complex equipment | Inability to accurately assess the true state of afterload, especially to reflect changes in the elasticity of the arterial system |
| Myocardial contractility | ||
| Ees | A direct indicator of myocardial contractility Can be accurately measured by pressure-volume loops | Requires invasive equipment and has limited clinical application Does not assess myocardial properties (only "ventricular" properties) Measurement complexity Little validation of single beat non-invasive methods beyond original derivation studies |
| Maximum left ventricular pressure | A direct measure of cardiac contractility and provides an assessment of LV function during systole Can be used to analyze patients with impaired cardiac function, especially those with hypertension and HF Provide personalized LVAC prediction and treatment recommendations | Requires invasive testing equipment (cardiac catheterization) and cannot be routinely applied clinically Only provides information on the highest pressure and does not fully reflect the dynamics of the entire systolic period |
| Maximum rate of left ventricular pressure change (dP/dt) | Reflects the strength of myocardial contraction capacity, which is a direct indicator of cardiac contractile function Dynamically reflects the performance of myocardial contraction in the early stages, suitable for real-time monitoring | Sensitive to preload and afterload, need to combine with other indicators to comprehensively assess cardiac function |
| EF | Non-invasive and suitable for a wide range of clinical settings | Insensitivity to subtle changes in myocardial contractility |
| [1] |
Sagawa K, Lie RK, Schaefer J. Translation of Otto Frank's paper "die grundform des arteriellen pulses" zeitschrift für biologie 37: 483-526 (1899). J Mol Cell Cardiol 1990; 22:253-254.
doi: 10.1016/0022-2828(90)91459-k pmid: 2192068 |
| [2] |
Suga H, Sagawa K. Instantaneous pressure-volume relationships and their ratio in the excised, supported canine left ventricle. Circ Res 1974; 35:117-126.
doi: 10.1161/01.res.35.1.117 pmid: 4841253 |
| [3] |
Sunagawa K, Sagawa K, Maughan WL. Ventricular interaction with the loading system. Ann Biomed Eng 1984; 12:163-189.
pmid: 6507965 |
| [4] | Sunagawa K, Maughan WL, Burkhoff D, Sagawa K. Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol 1983; 245:H773-H780. |
| [5] |
Ikonomidis I, Aboyans V, Blacher J, Brodmann M, Brutsaert DL, Chirinos JA, et al. The role of ventricular-arterial coupling in cardiac disease and heart failure: assessment, clinical implications and therapeutic interventions. a consensus document of the European Society of Cardiology Working Group on Aorta & Peripheral Vascular Diseases, European Association of Cardiovascular Imaging, and Heart Failure Association. Eur J Heart Fail 2019; 21:402-424.
doi: 10.1002/ejhf.1436 pmid: 30859669 |
| [6] | Chantler PD, Lakatta EG. Arterial-ventricular coupling with aging and disease. Front Physiol 2012; 7:90. |
| [7] |
Sunagawa K, Maughan WL, Sagawa K. Optimal arterial resistance for the maximal stroke work studied in isolated canine left ventricle. Circ Res 1985; 56:586-595.
pmid: 3978773 |
| [8] | Burkhoff D, Sagawa K. Ventricular efficiency predicted by an analytical model. Am J Physiol 1986; 250:R1021-R1027. |
| [9] |
Kelly RP, Ting CT, Yang TM, Liu CP, Maughan WL, Chang MS, et al. Effective arterial elastance as index of arterial vascular load in humans. Circulation 1992; 86:513-521.
doi: 10.1161/01.cir.86.2.513 pmid: 1638719 |
| [10] | Chirinos JA. Ventricular-arterial coupling: invasive and non-invasive assessment. Artery Res 2013; 7:2. |
| [11] |
Pinsky MR, Guarracino F. Pathophysiological implications of ventriculoarterial coupling in septic shock. Intensive Care Med Exp 2023; 11:87.
doi: 10.1186/s40635-023-00573-9 pmid: 38062332 |
| [12] |
Kass DA, Kelly RP. Ventriculo-arterial coupling: concepts, assumptions, and applications. Ann Biomed Eng 1992; 20:41-62.
pmid: 1562104 |
| [13] | Kosova E, Ricciardi M. Cardiac Catheterization. JAMA 2017; 13:2344. |
| [14] |
Monge García MI, Jian Z, Hatib F, Settels JJ, Cecconi M, Pinsky MR. Dynamic arterial elastance as a ventriculo-arterial coupling index: an experimental animal study. Front Physiol 2020; 11:284.
doi: 10.3389/fphys.2020.00284 pmid: 32327999 |
| [15] |
Safar ME. Arterial stiffness as a risk factor for clinical hypertension. Nat Rev Cardiol 2018; 15:97-105.
doi: 10.1038/nrcardio.2017.155 pmid: 29022570 |
| [16] | O'Rourke MF, Pauca A, Jiang XJ. Pulse wave analysis. Br J Clin Pharmacol 2001; 51:507-522. |
| [17] |
Zhang Y, Lacolley P, Protogerou AD, Safar ME. Arterial stiffness in hypertension and function of large arteries. Am J Hypertens 2020; 33:291-296.
doi: 10.1093/ajh/hpz193 pmid: 32060496 |
| [18] |
Chirinos JA. Arterial stiffness: basic concepts and measurement techniques. J Cardiovasc Transl Res 2012; 5:243-255.
doi: 10.1007/s12265-012-9359-6 pmid: 22447229 |
| [19] |
Chen CH, Fetics B, Nevo E, Rochitte CE, Chiou KR, Ding PA, et al. Noninvasive single-beat determination of left ventricular end-systolic elastance in humans. J Am Coll Cardiol 2001; 38:2028-2034.
pmid: 11738311 |
| [20] |
Evangelista A, Flachskampf F, Lancellotti P, Badano L, Aguilar R, Monaghan M, et al. European association of echocardiography recommendations for standardization of performance, digital storage and reporting of echocardiographic studies. Eur J Echocardiogr 2008; 9:438-448.
doi: 10.1093/ejechocard/jen174 pmid: 18579482 |
| [21] |
Adji A, Kachenoura N, Bollache E, Avolio AP, O'Rourke MF, Mousseaux E. Magnetic resonance and applanation tonometry for noninvasive determination of left ventricular load and ventricular vascular coupling in the time and frequency domain. J Hypertens 2016; 34:1099-1108.
doi: 10.1097/HJH.0000000000000925 pmid: 27054528 |
| [22] | Asadi H, Hedayat M, Borazjani I. The effects of implantation orientation of a bileaflet mechanical heart valve in an anatomic left ventricle-aorta configuration. J Biomech Eng 2022; 144:101008. |
| [23] |
Schäfer M, Younoszai A, Truong U, Browne LP, Mitchell MB, Jaggers J, et al. Influence of aortic stiffness on ventricular function in patients with Fontan circulation. J Thorac Cardiovasc Surg 2019; 157:699-707.
doi: S0022-5223(18)32543-1 pmid: 30396734 |
| [24] | Trambaiolo P, Figliuzzi I, Salvati M, Bertini P, Brizzi G, Tocci G, et al. Ventriculo-arterial coupling in the intensive cardiac care unit: a non-invasive prognostic parameter. Int J Cardiol 2022; 348:85-89. |
| [25] | Mihaileanu S, Antohi EL. Revisiting the relationship between left ventricular ejection fraction and ventricular-arterial coupling. ESC Heart Fail 2020; 7:2214-2222. |
| [26] | Sanchez-Martinez S, Duchateau N, Erdei T, Kunszt G, Aakhus S, Degiovanni A, et al. Machine learning analysis of left ventricular function to characterize heart failure with preserved ejection fraction. Circ Cardiovasc Imaging 2018; 11:e007138. |
| [27] |
Krittanawong C, Johnson KW, Rosenson RS, Wang Z, Aydar M, Baber U, et al. Deep learning for cardiovascular medicine: a practical primer. Eur Heart J 2019; 40:2058-2073.
doi: 10.1093/eurheartj/ehz056 pmid: 30815669 |
| [28] | Pagoulatou S, Rommel KP, Kresoja KP, von Roeder M, Lurz P, Thiele H, et al. In vivo application and validation of a novel noninvasive method to estimate the end-systolic elastance. Am J Physiol Heart Circ Physiol 2021; 320:H1554-H1564. |
| [29] | Gamarra A, Díez-Villanueva P, Salamanca J, Aguilar R, Mahía P, Alfonso F. Development and clinical application of left ventricular-arterial coupling non-invasive assessment methods. J Cardiovasc Dev Dis 2024; 11:141. |
| [30] | Wu L, Zhang M, Chen J, Jin L, Shen C, Sun J, et al. A novel index system for assessing ventricular-vascular coupling. Rev Cardiovasc Med 2023; 24:282. |
| [31] | Saeed S, Holm H, Nilsson PM. Ventricular-arterial coupling: definition, pathophysiology and therapeutic targets in cardiovascular disease. Expert Rev Cardiovasc Ther 2021; 19:753-761. |
| [32] | Rocha E. Velocidade da onda de pulso arterial: um marcador da rigidez arterial e a sua aplicabilidade na prática clínica [pulse wave velocity: a marker of arterial stiffness and its applicability in clinical practice]. Rev Port Cardiol 2011; 30:699-702. |
| [33] |
Lin Jin, Xinyi Li, Mengjiao Zhang, Xujie Zhang, Chaoyu Xian, Fuyou Liang, et al. Arterial stiffness and cardiovascular risk: the role of brachial cuff-measured index. Advanced Ultrasound in Diagnosis and Therapy 2023; 7:348-355.
doi: 10.37015/AUDT.2023.230045 |
| [34] | Kažukauskienė I, Balčiūnaitė G, Baltrūnienė V, Čelutkienė J, Maneikienė VV, Čibiras S, et al. Left ventricular global longitudinal strain predicts elevated cardiac pressures and poor clinical outcomes in patients with non-ischemic dilated cardiomyopathy. Cardiovasc Ultrasound 2021; 19:21. |
| [35] | Krishnasamy R, Isbel NM, Hawley CM, Pascoe EM, Burrage M, Leano R, et al. Left ventricular global longitudinal strain (gls) is a superior predictor of all-cause and cardiovascular mortality when compared to ejection fraction in advanced chronic kidney disease. PLoS One 2015; 10:e0127044. |
| [36] |
Pietri P, Stefanadis C. Cardiovascular aging and longevity: JACC state-of-the-art review. J Am Coll Cardiol 2021; 77:189-204.
doi: 10.1016/j.jacc.2020.11.023 pmid: 33446313 |
| [37] |
Redfield MM, Jacobsen SJ, Borlaug BA, Rodeheffer RJ, Kass DA. Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation 2005; 112:2254-2262.
doi: 10.1161/CIRCULATIONAHA.105.541078 pmid: 16203909 |
| [38] |
Coutinho T. Arterial stiffness and its clinical implications in women. Can J Cardiol 2014; 30:756-764.
doi: 10.1016/j.cjca.2014.03.020 pmid: 24970788 |
| [39] |
Gebhard C, Stähli BE, Gebhard CE, Tasnady H, Zihler D, Wischnewsky MB, et al. Age- and gender-dependent left ventricular remodeling. Echocardiography 2013; 30:1143-1150.
doi: 10.1111/echo.12264 pmid: 23742210 |
| [40] |
Borlaug BA, Lam CS, Roger VL, Rodeheffer RJ, Redfield MM. Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction. J Am Coll Cardiol 2009; 54:410-418.
doi: 10.1016/j.jacc.2009.05.013 pmid: 19628115 |
| [41] | Leancă SA, Crișu D, Petriș AO, Afrăsânie I, Genes A, Costache AD, et al. Left ventricular remodeling after myocardial infarction: from physiopathology to treatment. Life (Basel) 2022; 12:1111. |
| [42] | Seki H, Katayama K, Sakai H, Yonezawa T, Kunichika H, Saeki Y, et al. Effect of dobutamine of ventriculoarterial coupling in acute regional myocardial ischemia in dogs. Am J Physiol 1996; 270:H1279-H1286. |
| [43] | Antohi EL, Chioncel O, Mihaileanu S. Overcoming the limits of ejection fraction and ventricular-arterial coupling in heart failure. Front Cardiovasc Med 2022; 8:750965. |
| [44] |
Tomoto T, Sugawara J, Hirasawa A, Imai T, Maeda S, Ogoh S. Impact of short-term training camp on arterial stiffness in endurance runners. J Physiol Sci 2015; 65:445-449.
doi: 10.1007/s12576-015-0383-6 pmid: 26037815 |
| [45] | Zhang X, Zhao Y, Guo D, Luo M, Zhang Q, Zhang L, et al. Exercise improves heart function after myocardial infarction: the merits of AMPK. Cardiovasc Drugs Ther 2024. |
| [46] | Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA, et al. American college of sports medicine position stand. exercise and hypertension. Med Sci Sports Exerc 2004; 36:533-553. |
| [47] | Qi J, Zhou S, Wang G, Hua R, Wang X, He J, et al. The antioxidant dendrobium officinale polysaccharide modulates host metabolism and gut microbiota to alleviate high-fat diet-induced atherosclerosis in ApoE-/- Mice. Antioxidants (Basel) 2024; 13:599. |
| [48] | Bailén Almorox R. Prevención primaria de la enfermedad cardiovascular con una dieta mediterránea [cardiovascular disease primary prevention with a mediterranean diet]. Rev Clin Esp (Barc) 2013; 213:355-356. |
| [49] |
Osranek M, Eisenach JH, Khandheria BK, Chandrasekaran K, Seward JB, Belohlavek M. Arterioventricular coupling and ventricular efficiency after antihypertensive therapy: a noninvasive prospective study. Hypertension 2008; 51:275-281.
pmid: 18158354 |
| [50] |
Shimizu G, Hirota Y, Kita Y, Kawamura K, Saito T, Gaasch WH. Left ventricular midwall mechanics in systemic arterial hypertension. myocardial function is depressed in pressure-overload hypertrophy. Circulation 1991; 83:1676-1684.
pmid: 1827056 |
| [51] |
Melenovsky V, Borlaug BA, Rosen B, Hay I, Ferruci L, Morell CH, et al. Cardiovascular features of heart failure with preserved ejection fraction versus nonfailing hypertensive left ventricular hypertrophy in the urban baltimore community: the role of atrial remodeling/dysfunction. J Am Coll Cardiol 2007; 49:198-207.
doi: 10.1016/j.jacc.2006.08.050 pmid: 17222731 |
| [52] |
Aurigemma GP, Silver KH, Priest MA, Gaasch WH. Geometric changes allow normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. J Am Coll Cardiol 1995; 26:195-202.
doi: 10.1016/0735-1097(95)00153-q pmid: 7797752 |
| [53] |
de Simone G, Devereux RB, Roman MJ, Ganau A, Saba PS, Alderman MH, et al. Assessment of left ventricular function by the midwall fractional shortening/end-systolic stress relation in human hypertension. J Am Coll Cardiol 1994; 23:1444-1451.
pmid: 8176105 |
| [54] |
Lam CS, Shah AM, Borlaug BA, Cheng S, Verma A, Izzo J, et al. Effect of antihypertensive therapy on ventricular-arterial mechanics, coupling, and efficiency. Eur Heart J 2013; 34:676-683.
doi: 10.1093/eurheartj/ehs299 pmid: 22963833 |
| [55] |
Chirinos JA, Sweitzer N. Ventricular-arterial coupling in chronic heart failure. Card Fail Rev 2017; 3:12-18.
doi: 10.15420/cfr.2017:4:2 pmid: 28785470 |
| [56] | Scarlatescu AI, Micheu MM, Petre IG, Oprescu N, Mihail AM, Cojocaru ID, et al. Left ventricular-arterial coupling as an independent predictor of adverse events in young patients with st elevation myocardial infarction-a 3d echocardiographic study. Biomedicines 2024; 12:105. |
| [57] |
Kolh P, Lambermont B, Ghuysen A, D'Orio V, Gerard P, Morimont P, et al. Alteration of left ventriculo-arterial coupling and mechanical efficiency during acute myocardial ischemia. Int Angiol 2003; 22:148-158.
pmid: 12865880 |
| [58] |
Fretheim A, Odgaard-Jensen J, Brørs O, Madsen S, Njølstad I, Norheim OF, et al. Comparative effectiveness of antihypertensive medication for primary prevention of cardiovascular disease: systematic review and multiple treatments meta-analysis. BMC Med 2012; 10:33.
doi: 10.1186/1741-7015-10-33 pmid: 22480336 |
| [59] |
Schettini IVG, Rios DRA, Figueiredo RC. Effect of different classes of antihypertensive drugs on arterial stiffness. Curr Hypertens Rep 2023; 25:61-70.
doi: 10.1007/s11906-023-01238-4 pmid: 36892734 |
| [60] |
Suchard MA, Schuemie MJ, Krumholz HM, You SC, Chen R, Pratt N, et al. Comprehensive comparative effectiveness and safety of first-line antihypertensive drug classes: a systematic, multinational, large-scale analysis. Lancet 2019; 394:1816-1826.
doi: S0140-6736(19)32317-7 pmid: 31668726 |
| [61] | Yoon HM, Joo SJ, Boo KY, Lee JG, Choi JH, Kim SY, et al. Impact of cardiac rehabilitation on ventricular-arterial coupling and left ventricular function in patients with acute myocardial infarction. PLoS One 2024; 19:e0300578. |
| [62] | Timor-Tritsch IE, Platt LD. Three-dimensional ultrasound experience in obstetrics. Curr Opin Obstet Gynecol 2002; 14:569-575. |
| [63] | Blaas HG, Eik-Nes SH, Kiserud T, Berg S, Angelsen B, Olstad B. Three-dimensional imaging of the brain cavities in human embryos. Ultrasound Obstet Gynecol 1995; 5:228-232. |
| [64] | Feichtinger W. Transvaginal three-dimensional imaging. Ultrasound Obstet Gynecol 1993; 3:375-378. |
| [65] |
Steiner H, Gregg AR, Bogner G, Graf AH, Weiner CP, Staudach A. First trimester three-dimensional ultrasound volumetry of the gestational sac. Arch Gynecol Obstet 1994; 255:165-170.
pmid: 7695361 |
| [66] |
Ding CCA, Dokos S, Bakir AA, Zamberi NJ, Liew YM, Chan BT, et al. Simulating impaired left ventricular-arterial coupling in aging and disease: a systematic review. Biomed Eng Online 2024; 23:24.
doi: 10.1186/s12938-024-01206-2 pmid: 38388416 |
| [67] |
Gao Y, Jiang YN, Shi R, Guo YK, Xu HY, Min CY, et al. Effects of diabetes mellitus on left ventricular function and deformation in patients with restrictive cardiomyopathies: a 3.0T CMR feature tracking study. Cardiovasc Diabetol 2023; 22:317.
doi: 10.1186/s12933-023-02033-w pmid: 37985989 |
| [68] | Yang Y, Deng W, Wang Y, Li T, Chen Y, Long C, et al. The effect of omega-3 fatty acids and its combination with statins on lipid profile in patients with hypertriglyceridemia: a systematic review and meta-analysis of randomized controlled trials. Front Nutr 2022; 9:1039056. |
| [69] |
Sagawa K. The end-systolic pressure-volume relation of the ventricle: definition, modifications and clinical use. Circulation 1981; 63:1223-1227.
pmid: 7014027 |
| [70] | Masutani S, Senzaki H. Assessment of ventricular function using the pressure-volume relationship. Springer Japan 2015:97-126. |
| [71] | Yerebakan C, Klopsch C, Prietz S, Boltze J, Vollmar B, Liebold A, et al. Pressure-volume loops: feasible for the evaluation of right ventricular function in an experimental model of acute pulmonary regurgitation? Interact Cardiovasc Thorac Surg 2009; 9:163-168. |
| [72] | Sequí-Domínguez I, Cavero-Redondo I, Álvarez-Bueno C, Pozuelo-Carrascosa DP, Nuñez de Arenas-Arroyo S, Martínez-Vizcaíno V. Accuracy of pulse wave velocity predicting cardiovascular and all-cause mortality. a systematic review and meta-analysis. J Clin Med 2020; 9:2080. |
| [73] | Prelević V, Jelaković A, Gašparović K. Different methods for measurements and estimation of pulse wave velocity are not interchangeable. Artery Res 2024; 30:16. |
| [74] | Stephane Laurenta, John Cockcroftb, Pierre Boutouyriea, Cristina Giannattasiod, Daniel Hayoz. Abridged version of the expert consensus document on arterial stiffness. Artery Research 2007; 1:2-12. |
| [75] |
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. European network for non-invasive investigation of large arteries. expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27:2588-2605.
doi: 10.1093/eurheartj/ehl254 pmid: 17000623 |
| [76] | Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015; 28:1-39. |
| [77] | Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the european association of cardiovascular imaging. J Am Soc Echocardiogr 2016; 29:277-314. |
| [1] | Yang Yun, Zhang Xin, Zhang Ruize, Jiang Jingrong, Xie Yuji, Fang Lingyun, Zhang Jing, Xie Mingxing, Wang Jing. Current Status and Progress in Arterial Stiffness Evaluation: A Comprehensive Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 172-182. |
| [2] | Zhang Xin, Yang Yun, Zhang Ruize, Zhang Linyue, Xie Yuji, Wu Wenqian, Zhang Jing, Lv Qing, Wang Jing, Xie Mingxing. Noninvasive Evaluation of Left Ventricular-Arterial Coupling: Methodologies and Clinical Relevance [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 149-158. |
| [3] | Chen Ya, Wang Xinqi, Chen Anni, Li Zhenyi, Yang Lan, Li Zhaojun, Jin Lin, Wang Xifu. The Application and Research Progress of Cardiac Magnetic Resonance in the Assessment of Right Ventricular-Pulmonary Arterial Coupling [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 183-194. |
| [4] | Li Zhenyi, Chen Ya, Wang Xinqi, Yang Lan, Chen Anni, Li Zhaojun, Jin Lin. Left and Right Ventricular Interaction: Insight from Echocardiography Imaging [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 195-204. |
| [5] | Wang Xinqi, Chen Anni, Yang Lan, Chen Ya, Li Zhenyi, Li Zhaojun, Jin Lin. Evaluation Methods and Progress of Right Ventricular-pulmonary Artery Coupling [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 205-216. |
| [6] | Junrong Hong, MD, Pingyang Zhang, MD, PhD, Mengyao Fei, MD, Lingling Wang, MD. A Study on Left Atrial Function in Patients with Essential Hypertension Using Four-Dimensional Echocardiography [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(2): 64-73. |
| [7] | Lin Jin, MD, Xinyi Li, BS, Mengjiao Zhang, MS, Xujie Zhang, BS, Chaoyu Xian, BS, Fuyou Liang, PhD, Zhaojun Li, MD. Arterial Stiffness and Cardiovascular Risk: The Role of Brachial Cuff-measured Index [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(4): 348-355. |
| [8] | Rifei Li, MM, Yuanmei Zhang, MM, Chengkai Zhang, MM, Xuenian Huang, MM, Shangwei Ding, MD. Contrast Echocardiography Evaluation of Microcirculation of Myocardial Infarction Caused by Takotsubo Syndrome: Case Report and Literature Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(3): 258-261. |
| [9] | Jianping Xu, MS, Faping Cui, MS, Shuixiu Dou, MS, Jiafu Ou, MD. Echocardiography of Marfan's Syndrome Patient with New Gene Mutation of FBN1 with 13-year Follow-up [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(3): 249-253. |
| [10] | Xiaoxue Chen, MD, Shaoling Yang, PhD, Qianqian He, MD, Yin Wang, PhD, Linyan Fan, MD, Fengling Wang, MD, Kun Zhao, MD, Jing Hu, MD. Automated Measurements of Left Ventricular Ejection Fraction and Volumes Using the EchoPAC System [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(3): 226-235. |
| [11] | Yichen Qu, MD, Ya Yang, MD, Jinjie Xie, MD, Rongjuan Li, MD, Han Zhang, MD, Li Song, MD, Yueli Wang, MD, Jing Li, MD. Incomplete Shone’s Complex with BAV and VSD in Adult Diagnosed by Echocardiography [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(2): 106-108. |
| [12] | Ting Sun, MD, Guoliang Lu, MD, Jian Fang, MD, Shaobo Xie, MD. Silent Embolization Following Hybrid Device Closure of Atrial Septal Defect [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(4): 352-353. |
| [13] | Ting Sun, MD, Guoliang Lu, MD, Jian Fang, MD, Shaobo Xie, MD. Transthoracic Echocardiography for Evaluation of an Intrapulmonary Artery Mass [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(4): 329-334. |
| [14] | Luwen Liu, MS, Shaobo Duan, MD, Yaqiong Li, PhD, Ruiqing Liu, MD, Yuejin Wu, MS, Lianzhong Zhang, MD. Development Status and Prospect of Remote Diagnosis and Treatment of Echocardiography Worldwide [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(4): 303-307. |
| [15] | Huan Cen, MS, Jinhua Li, MD, Bijing Li, MS, Pengtao Sun, MS. Two- and Three-Dimensional Echocardiography for Primary Cardiac Lymphomas: A Case Report and Literature Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(3): 255-259. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
Share: WeChat
Copyright ©2018 Advanced Ultrasound in Diagnosis and Therapy
|
 Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
