Advanced Ultrasound in Diagnosis and Therapy ›› 2025, Vol. 9 ›› Issue (2): 127-137.doi: 10.37015/AUDT.2024.240014
• Review Articles • Previous Articles Next Articles
Ye Beibeia,b, Zhang Yifenga,b,c,*( )
)
Received:2024-06-04
Revised:2024-05-14
Accepted:2024-06-12
Online:2025-06-30
Published:2025-07-06
Contact:
Department of Medical Ultrasound, Shanghai Tenth People’s Hopital, School of Medicine, Tongji University, Shanghai 200072, China; Ultrasound Research and Education Institute, Clinical Research Center Interventional Medicine, School of Medicine, Tongji University, Shanghai, China; Shanghai Engineering Research Center of Ultrasound Diagnosis and Treatment, Shanghai, China. e-mail: Ye Beibei, Zhang Yifeng. Preoperative Diagnosis of Thyroid Follicular Tumor. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 127-137.
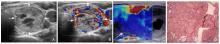
Figure 2
Images of a 45-year-old man with follicular thyroid carcinoma. (A) Grey scale ultrasound: a hemerogeneous hypo-/mixechoic mass with clear margin, regular shape and no calcification, the lesion was wider than taller (arrows); (B) CDFI: the blood flow signals in and para-tumor was rich (arrows). (C) Elastic imaging: when the tumor infiltrates to the peripheral, the interior of the tumor was blue and the peripheral is colored, which means the internal structure was softer than the surrounding structure (arrows); (D) Postoperative pathology: under the microscope, numerous heteromorphic follicle epithelial cells could be seen. It was diagnosed as FTC."
Table 1
Comparison of follicular carcinoma and follicular adenoma of thyroid"
| Characteristic | Follicular thyroid carcinoma | Follicular thyroid adenoma |
|---|---|---|
| Composition | Predominantly solid [ | Solid or mixed cystic and solid [ |
| Echogenicity | Predominantly Hypoechoic [ | Iso or Hypoechoic [ |
| Echo texture | Heterogeneous [ | Predominantly homogeneous [ |
| Margin | Irregular or extra thyroidal extension [ | Smooth [ |
| Peripheral halo | Incomplete/unevenly thick [ | Present and thin [ |
| Vascularity | Rich internal flow [ | Peripheral flow [ |
| Metastasis | Hematogenous/lymphatic metastasis [ | No metastasis [ |
| Vascular and capsule | Invasion [ | No invasion [ |
Table 2
Comparison of thyroid follicular carcinoma and papillary thyroid carcinoma"
| Characteristic | Follicular thyroid carcinoma | Papillary thyroid carcinoma |
|---|---|---|
| Maximum diameter | Large diameter, mostly > 4 cm [ | Small diameter, mostly < 2 cm, predominantly in PTMC [ |
| Composition | Predominantly solid [ | Predominantly solid [ |
| Echogenicity | Predominantly Hypoechoic [ | Hypo or markedly Hypoechoic [ |
| Shape | Wider than tall [ | Taller than wide [ |
| Margin | Irregular or extra thyroidal extension [ | Lobulated or irregular or extra thyroidal extension [ |
| Calcification | Macrocalcifications [ | Punctate echogenic foci [ |
| Peripheral halo | Incomplete/unevenly thick [ | No peripheral halo [ |
| Vascularity | Rich internal flow [ | Atypical flow presentation [ |
| Metastasis | Hematogenous/lymphatic metastasis [ | Cervical lymphatic metastasis [ |
| BRAF V600E tests | Negative [ | Positive (60%~80%) [ |
| Pathology | Vascular and capsule invasion [ | Papillary features, glass changes in nucleus, psammoma bodies [ |
Table 3
Comparison of the characteristics of contrast-enhanced ultrasonography between follicular thyroid carcinoma, follicular thyroid adenoma and papillary thyroid carcinoma"
| Characteristic | Follicular thyroid carcinoma | Follicular thyroid adenoma | Papillary thyroid carcin oma |
|---|---|---|---|
| Boundary of the enhanced lesions | Ill-defined [ | Well-defined, ring-enhancement [ | Ill-defined [ |
| Enhancement homogeneity | Heterogeneous [ | Heterogeneous/Homogeneous [ | Heterogeneous [ |
| Size of the enhanced lesions | Lager than grey scale image [ | Similar to grey scale image size [ | Smaller than grey scale image [ |
| Enhancement degree | Hyper-/iso-enhancement [ | Hyperenhancement [ | Hypo/iso-enhancement [ |
| Enhancment direction | Centrifugal [ | Centripetal [ | Centripetal [ |
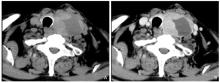
Figure 3
Images of an 84 years old man with follicular thyroid carcinoma. (A) Plain CT scan: the left lobe of thyroid gland was a lession with inhomogeneous low density, and the trachea is compressed and displaced (arrows); (B) Contrast enhancement CT scan: the early stage showed uneven enhancement. The boundary with surrounding tissues was unclear (arrows)."
| [1] | Baloch ZW, Asa SL, Barletta JA, Ghossein RA, Juhlin CC, Jung CK, et al. Overview of the 2022 WHO classification of thyroid neoplasms. Endocr Pathol 2022;33:27-63. |
| [2] |
Rossi ED, Adeniran AJ, Faquin WC. Pitfalls in thyroid cytopathology. Surg Pathol Clin 2019; 12:865-881.
doi: S1875-9181(19)30057-1 pmid: 31672295 |
| [3] | Uçan B, Şahin M, Önal B, Kızılgül M, Düğer H, Sencar ME, et al. Assessment of diagnostic value of preoperative elastography in thyroid nodules having indeterminate cytology results. Turk J Med Sci 2021;51:2924-2930. |
| [4] | Na HY, Moon JH, Choi JY, Yu HW, Jeong WJ, Kim YK, et al. Preoperative diagnostic categories of fine needle aspiration cytology for histologically proven thyroid follicular adenoma and carcinoma, and Hurthle cell adenoma and carcinoma: analysis of cause of under- or misdiagnoses. PLoS One 2020;15:e0241597. |
| [5] | Jainulabdeen T, Ramaswamy B, Devaraja K, Paruthikunnan SM, Bhandarkar AM. Preoperative staging of differentiated thyroid carcinomas: comparison of USG and CT with intraoperative findings and histopathology. Indian J Otolaryngol Head Neck Surg 2019;71:327-333. |
| [6] | Li Y, Jin C, Li J, Tong M, Wang M, Huang J, et al. Prevalence of thyroid nodules in China: a health examination cohort-based study. Front Endocrinol (Lausanne) 2021;12:676144. |
| [7] | Derwahl KM, Goretzki P. Schilddrüsenknoten: ATA-leitlinie aus europäischer sicht thyroid nodules: the guidelines of the american thyroid association from a european perspective. Dtsch Med Wochenschr 2020;145:1227-1235. |
| [8] | Davies L, Hoang JK. Thyroid cancer in the USA: current trends and outstanding questions. Lancet Diabetes Endocrinol 2021;9:11-12. |
| [9] | Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin 2021; 71:7-33. |
| [10] | Carling T, Udelsman R. Follicular neoplasms of the thyroid: what to recommend. Thyroid 2005;15:583-587. |
| [11] | Chung R, Guan H, Ponchiardi C, Cerda S, Marwaha N, Yilmaz OH, et al. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features: epidemiology and long-term outcomes in a strictly defined cohort. Thyroid 2021;31:68-75. |
| [12] | Elhassan MMA, Gismalla MDA, Mohamed SAH, Faggad A.Clinicopathological profile and management of thyroid carcinoma: a Sub-Saharan country experience. Thyroid Res 2023;16:35. |
| [13] | Ashorobi D, Lopez PP. Follicular Thyroid Cancer. In: StatPearls. StatPearls. Treasure Island (FL): StatPearls Publishing 2023. |
| [14] | Boucai L, Zafereo M, Cabanillas ME.Thyroid cancer: a review. JAMA. 2024;331:425-435. |
| [15] | Nilojan JS, Raviraj S, Madhuwantha UVP, Mathuvanthi T, Priyatharsan K.Metastatic thyroid follicular carcinoma presenting as pathological left clavicle fracture: an unusual skeletal metastasis at the time of diagnosis. Int J Surg Case Rep. 2024;114:109131. |
| [16] | Vuong HG, Le MK, Hassell L, Kondo T, Kakudo K.The differences in distant metastatic patterns and their corresponding survival between thyroid cancer subtypes. Int J Surg Case Rep. 2022;44:926-932. |
| [17] | Daniels GH. Follicular thyroid carcinoma: a perspective. Thyroid 2018;28:1229-1242. |
| [18] | Van Vlaenderen J, Logghe K, Schiettecatte E, Vermeersch H, Huvenne W, De Waele K, et al. A synchronous papillary and follicular thyroid carcinoma presenting as a large toxic nodule in a female adolescent. Int J Pediatr Endocrinol 2020;2020:14. |
| [19] | Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the american thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016;26:1-133. |
| [20] | Tay SY, Chen CY, Chan WP. Sonographic criteria predictive of benign thyroid nodules useful in avoiding unnecessary ultrasound-guided fine needle aspiration. J Formos Med Assoc 2015;114:590-597. |
| [21] | Huang Q, Xie L, Huang L, Wei W, Li H, Zhuang Y, et al. Development and validation of an ultrasonic diagnostic model for differentiating follicular thyroid carcinoma from follicular sdenoma. Int J Gen Med 2021;14:5069-5078. |
| [22] | de Jong MC, McNamara J, Winter L, Roskell D, Khan S, Mihai R. Risk of malignancy in thyroid nodules with indeterminate (THY3f) cytology. Ann R Coll Surg Engl 2022;104:703-709. |
| [23] | Oshita M, Ito Y, Miyamoto T, Ota H, Nakamura T, Hirokawa M, et al. Ultrasound findings of noninvasive follicular thyroid neoplasm with papillary-like nuclear features compared with those of follicular variant of papillary carcinoma and encapsulated papillary carcinoma: a single-institution study in Japan. Endocr J 2020;67:1147-1155. |
| [24] | Ou D, Yao J, Jin J, Yan M, Shi K, Zheng Q, et al. Ultrasonic identification and regression analysis of 294 thyroid follicular tumors. J Cancer Res Ther 2020;16:1056-1062. |
| [25] | Kuo TC, Wu MH, Chen KY, Hsieh MS, Chen A, Chen CN.Ultrasonographic features for differentiating follicular thyroid carcinoma and follicular adenoma. Asian J Surg 2020;43:339-346. |
| [26] | Li W, Song Q, Lan Y, Li J, Zhang Y, Yan L, et al. The value of sonography in distinguishing follicular thyroid carcinoma from adenoma. Cancer Manag Res 2021;13:3991-4002. |
| [27] | Ahn HS, Kim HS, Hong MJ.Ultrasonographic and cytologic assessments of follicular neoplasms of the thyroid: predictive features differentiating follicular carcinoma from follicular adenoma. PLoS One 2022;17:e0271437. |
| [28] | Lai X, Jiang Y, Zhang B, Liang Z, Jiang Y, Li J, et al. Preoperative sonographic features of follicular thyroid carcinoma predict biological behavior: a retrospective study. Medicine (Baltimore) 2018;97:e12814. |
| [29] | Lloret J, Ganado T, Subhi I, Familiar C, Moreno L, Suárez P, et al. An attempt to reduce unnecessary surgical procedures... Can ultrasound characteristics help in differentiating adenoma vs carcinoma in follicular thyroid neoplasms? Radiologia (Engl Ed) 2023;65:22-31. |
| [30] | Sillery JC, Reading CC, Charboneau JW, Henrichsen TL, Hay ID, Mandrekar JN. Thyroid follicular carcinoma: sonographic features of 50 cases. AJR Am J Roentgenol 2010;194:44-54. |
| [31] | Zheng Y, Zhang Y, Lu K,Wang J, Li L, Xu D, et al. Diagnostic value of an interpretable machine learning model based on clinical ultrasound features for follicular thyroid carcinoma. Quant Imaging Med Surg 2024;14:6311-6324. |
| [32] | Kim BK, Choi YS, Kwon HJ, Lee JS, Heo JJ, Han YJ, et al. Relationship between patterns of calcification in thyroid nodules and histopathologic findings. Endocr J 2013;60:155-160. |
| [33] | Zhang F, Mei F, Chen W, Zhang Y. Role of Ultrasound and Ultrasound-Based Prediction Model in Differentiating Follicular Thyroid Carcinoma From Follicular Thyroid Adenoma. J Ultrasound Med 2024;43:1389-1399. |
| [34] | Kobayashi K, Fujimoto T, Ota H, Hirokawa M, Yabuta T, Masuoka H, et al. Calcifications in thyroid tumors on ultrasonography: calcification types and relationship with histopathological type. Ultrasound Int Open2018;4:E45-E51. |
| [35] | Jeong SH, Hong HS, Lee EH.Can nodular hyperplasia of the thyroid gland be differentiated from follicular adenoma and follicular carcinoma by ultrasonography? Ultrasound Q 2016;32:349-355. |
| [36] | Saito D, Nakajima R, Yasuda S. Examination of malignant findings of thyroid nodules using thyroid ultrasonography. Journal of clinical medicine research 2022;12:499-507. |
| [37] | Rago T, Scutari M, Loiacono V, Santini F, Tonacchera M, Torregrossa L, et al. Low elasticity of thyroid nodules on ultrasound elastography is correlated with malignancy, degree of fibrosis, and high expression of galectin-3 and fibronectin-1. Thyroid 2017;27:103-110. |
| [38] | Ippolito D, Galimberti S, Leni D, Vacirca F, Nasr A, Bragazzi NL, et al. Use of shear wave elastography in the sonographic triage of thyroid nodules: feasibility study in a series of lesions already selected for fine needle aspiration. J Ultrasound Med 2019;38:1713-1720. |
| [39] | Anvari A, Dhyani M, Stephen AE, Samir AE. Reliability of shear-wave elastography estimates of the young modulus of tissue in follicular thyroid neoplasms. AJR Am J Roentgenol 2016;206:609-616. |
| [40] | Li Ning, Yang Lichun, Wang Liwei, Ding Lin. Ultrasonic radio-elastography combined with contrast-enhanced ultrasound in the diagnosis of thyroid follicular neoplasms. Radiology practice 2020;35:663-667. |
| [41] | Samir AE, Dhyani M, Anvari A, Prescott J, Halpern EF, Faquin WC, et al. Shear-wave elastography for the preoperative risk stratification of follicular-patterned lesions of the thyroid: diagnostic accuracy and optimal measurement plane. Radiology 2015;277:565-573. |
| [42] | Nell S, Kist JW, Debray TP, de Keizer B, van Oostenbrugge TJ, Borel Rinkes IH, et al. Qualitative elastography can replace thyroid nodule fine-needle aspiration in patients with soft thyroid nodules. A systematic review and meta-analysis. Eur J Radio 2015;84:652-661. |
| [43] | Bojunga J, Herrmann E, Meyer G, Weber S, Zeuzem S, Friedrich-Rust M. Real-time elastography for the differentiation of benign and malignant thyroid nodules: a meta-analysis. Thyroid 2010;20:1145-1150. |
| [44] | Xi X, Gao L, Wu Q, Fang S, Xu J, Liu R, et al. Differentiation of thyroid nodules difficult to diagnose with contrast-enhanced ultrasonography and real-time elastography. Front Oncol 2020;10:112. |
| [45] | Zhang Y, Zhang MB, Luo YK, Li J, Wang ZL, Tang J.The value of peripheral enhancement pattern for diagnosing thyroid cancer using contrast-enhanced Ultrasound. Int J Endocrinol 2018;2018:1625958. |
| [46] | Wu Q, Qu Y, Li Y, Liu Y, Shen J, Wang Y. Logistic regression analysis of contrast-enhanced ultrasound and conventional ultrasound of follicular thyroid carcinoma and follicular adenoma. Gland Surg 2021;10:2890-2900. |
| [47] | Fan jm. Analysis of imaging characteristics of multi-slice spiral CT in diagnosis of thyroid carcinoma. Chin J minkang med 2020;32:94-96. |
| [48] | Weber AL, Randolph G, Aksoy FG. The thyroid and parathyroid glands. CT and MR imaging and correlation with pathology and clinical findings. Radiol Clin North Am 2020;38:1105-1129. |
| [49] | Wu JH, Zeng W, Wu RG, Wang M, Ye F, Fu MY.Comparison of ultrasonography and CT for determining the preoperative benign or malignant nature of thyroid nodules: diagnostic performance according to calcification. Technol Cancer Res Treat 2020;19:1533033820948183. |
| [50] | Yang TT, Huang Y, Jing XQ, Gai XJ, Li WW. CT-detected solitary thyroid calcification: an important imaging feature for papillary carcinoma. Onco Targets Ther 2016;9:6273-6279. |
| [51] | Makino T, Orita Y, Tachibana T, Marunaka H, Miki K, Akisada N, et al. Computed tomography findings for diagnosing follicular thyroid neoplasms. Acta Med Okayama 2018;72:577-581. |
| [52] | Gu Y, Han ZJ, Xu L, Pen Y, Wu J. The ultrasound differential diagnosis of papillary thyroid micro-carcinoma and micronodular goiter. Chinese Journal of Ultrasound in Medicine 2013;29:211-214. |
| [53] | Wang F, Ding H, Wang Q, Wen P. The osteopontin expression and microvascular density in thyroid cancer, comparison of CT and ultrasound in diagnosis of thyroid cancer and correlations of CT features and thyroid cancer. Minerva Endocrinol (Torino) 2022;47:388-394. |
| [54] | Lai XF, Shu YY, Han ZJ, Chen WH, Xiang JJ, Ding JW. Value of CT in the diagnosis and differential diagnosis of thyroid follicular nodule lesions. Journal of oncology 2013;19:470-475. |
| [55] | Han ZJ, Shu YY, Lai XF, Chen WH. Value of computed tomography in determining the nature of papillary thyroid microcarcinomas: evaluation of the computed tomographic characteristics. Clin Imaging 2013;37:664-668. |
| [56] | Wu Y, Yue X, Shen W, Du Y, Yuan Y, Tao X, et al. Diagnostic value of diffusion-weighted MR imaging in thyroid disease: application in differentiating benign from malignant disease. BMC Med Imaging 2013;13:23. |
| [57] | Hu S, Zhang H, Zhong Y, Agyekum EA, Sun Z, Ge Y, et al. Assessing diagnostic value of combining ultrasound and MRI in extrathyroidal extension of papillary thyroid carcinoma. Cancer Manag Res 2022;14:1285-1292. |
| [58] | Meyer HJ, Wienke A, Surov A. Discrimination between malignant and benign thyroid tumors by diffusion-weighted imaging - a systematic review and meta analysis. Magn Reson Imaging 2021;84:41-57. |
| [59] | Tang Q, Liu X, Jiang Q, Zhu L, Zhang J, Wu PY, et al. Unenhanced magnetic resonance imaging of papillary thyroid carcinoma with emphasis on diffusion kurtosis imaging. Quant Imaging Med Surg 2023;13:2697-2707. |
| [60] | Aghaghazvini L, Sharifian H, Yazdani N, Hosseiny M, Kooraki S, Pirouzi P, et al. Differentiation between benign and malignant thyroid nodules using diffusion-weighted imaging, a 3-T MRI study. Indian J Radiol Imaging 2018;28:460-464. |
| [61] | Song B, Zheng T, Wang H, Tang L, Xie X, Fu Q, et al. Prediction of follicular thyroid neoplasm and malignancy of follicular thyroid neoplasm using multiparametric MRI. J Imaging Inform Med 2024;37:2852-2864. |
| [62] | Hao Y, Pan C, Chen W, Li T, Zhu W, Qi J. Differentiation between malignant and benign thyroid nodules and stratification of papillary thyroid cancer with aggressive histological features: Whole-lesion diffusion-weighted imaging histogram analysis. J Magn Reson Imaging 2016;44:1546-1555. |
| [63] | Zhu X, Wang J, Wang YC, Zhu ZF, Tang J, Wen XW, et al. Quantitative differentiation of malignant and benign thyroid nodules with multi-parameter diffusion-weighted imaging. World J Clin Cases 2022;10:8587-8598. |
| [64] | Chung SR, Lee JH, Yoon RK, Sung TY, Song DE, Pfeuffer J, et al. Differentiation of follicular carcinomas from adenomas using histogram obtained from diffusion-weighted MRI. Clin Radiol 2020;75:878.e13-878.e19. |
| [65] | Ciappuccini R, Licaj I, Lasne-Cardon A, Babin E, de Raucourt D, Blanchard D, et al. 18F-fluorocholine positron emission tomography/computed tomography is a highly sensitive but poorly specific tool for identifying malignancy in thyroid nodules with indeterminate cytology: the chocolate study. Thyroid 2021;31:800-809. |
| [66] | Abou Karam G, Malhotra A.PET/CT may assist in avoiding pointless thyroidectomy in indeterminate thyroid nodules: a narrative review. Cancers (Basel) 2023;15:1547. |
| [67] | Vriens D, de Koster EJ, de Geus-Oei LF, Oyen WJG; EfFECTS trial consortium. Preoperative stratification of cytologically indeterminate thyroid nodules by [18F]FDG-PET: can Orpheus bring back Eurydice?. Eur J Nucl Med Mol Imaging 2023;50:975-979. |
| [68] | de Leijer JF, Metman MJH, van der Hoorn A, Brouwers AH, Kruijff S, van Hemel BM, et al. Focal thyroid incidentalomas on 18F-FDG PET/CT: a systematic review and meta-analysis on prevalence, risk of malignancy and inconclusive fine needle aspiration. Front Endocrinol (Lausanne) 2021;12:723394. |
| [69] | Sayiner ZA, Elboğa U, Sahin E, Ozturk S, Cayirli YB, Celen YZ, et al. Comparison of 68Ga-FAPI-04 and 18F-FDG PET/CT for diagnosis of metastatic lesions in patients with recurrent papillary thyroid carcinoma. Hell J Nucl Med 2023;26:41-46. |
| [70] | Terroir M, Caramella C, Borget I, Bidault S, Dromain C, El Farsaoui K, et al. F-18-Dopa positron emission tomography/computed tomography is more sensitive than whole-body magnetic resonance imaging for the localization of persistent/recurrent disease of medullary thyroid cancer patients. Thyroid 2019;29:1457-1464. |
| [71] | Zampella E, Klain M, Pace L, Cuocolo A. PET/CT in the management of differentiated thyroid cancer. Diagn Interv Imaging. 2021;102:515-523. |
| [72] | Jat MA. Comparison of surgeon-performed ultrasound-guided fine needle aspiration cytology with histopathological diagnosis of thyroid nodules. Pak J Med Sci 2019;35:1003-1007. |
| [73] | Ohori NP, Nishino M. Follicular neoplasm of thyroid revisited: current differential diagnosis and the impact of molecular testing. Adv Anat Pathol 2023;30:11-23. |
| [74] | Park KW, Shin JH, Hahn SY, Oh YL, Kim SW, Kim TH, et al. Ultrasound-guided fine-needle aspiration or core needle biopsy for diagnosing follicular thyroid carcinoma? Clin Endocrinol (Oxf) 2020;92:468-474. |
| [75] | Kim JY, Chang S, Kwon AY, Park EY, Kim TH, Choi S, et al. Core needle biopsy and ultrasonography are superior to fine needle aspiration in the management of follicular variant papillary thyroid carcinomas. Endocrine 2022;75:437-446. |
| [76] | Karatay E, Javadov M, Kaya H.Thyroid nodule core needle biopsy - current approach. Endokrynol Pol 2023;74. |
| [77] | Guan H, Toraldo G, Cerda S, Godley FA, Rao SR, McAneny D, et al. Utilities of RAS mutations in preoperative fine needle biopsies for decision making for thyroid nodule management: results from a single-center prospective cohort. Thyroid 2020;30:536-547. |
| [78] | Nikiforov YE, Nikiforova MN. Molecular genetics and diagnosis of thyroid cancer. Nat Rev Endocrinol 2017;7:569-580. |
| [79] | Fagin JA, Nikiforov YE. Progress in thyroid cancer genomics: a 40-year journey. Thyroid 2023;33:1271-1286. |
| [80] | Liu R, Xing M.TERT promoter mutations in thyroid cancer. Endocr Relat Cancer2016;23:R143-R155. |
| [81] | Li S, Xue J, Jiang K, Chen Y, Zhu L, Liu R.TERT promoter methylation is associated with high expression of TERT and poor prognosis in papillary thyroid cancer. Front Oncol 2024;14:1325345. |
| [82] | Pinto JO, Livhits MJ, Yeh MW, Kaykov A, Klopper JP, Kloos RT, et al. Histopathology of telomerase reverse transcriptase promoter (TERT) mutated indeterminate thyroid nodules. J Clin Transl Endocrinol 2023;35:100329. |
| [83] | Xing M. Genetic alterations in the phosphatidylinositol-3 kinase/Akt pathway in thyroid cancer. Thyroid 2010;20:697-706. |
| [84] | Santiago K, Chen Wongworawat Y, Khan S.Differential microRNA-signatures in thyroid cancer subtypes. J Oncol 2020;2020:2052396. |
| [85] | Depciuch J, Stanek-Widera A, Skrzypiec D, Lange D, Biskup-Frużyńska M, Kiper K, et al. Spectroscopic identification of benign (follicular adenoma) and cancerous lesions (follicular thyroid carcinoma) in thyroid tissues. J Pharm Biomed Anal 2019;170:321-326. |
| [86] | Rong Y, Torres-Luna C, Tuszynski G, Siderits R, Chang FN.Differentiating thyroid follicular adenoma from follicular carcinoma via G-protein coupled receptor-associated sorting protein 1 (GASP-1). Cancers (Basel)2023;15:3404. |
| [87] | Sun Y, Li L, Zhou Y, Ge W, Wang H, Wu R, et al. Stratification of follicular thyroid tumours using data-independent acquisition proteomics and a comprehensive thyroid tissue spectral library. Mol Oncol 2022;16:1611-1624. |
| [88] | Chen Z, Lin Y, Lai S, Wang P, Li J, Wang L, et al. The utility of serum anti-thyroglobulin antibody and thyroglobulin in the preoperative differential diagnosis of thyroid follicular neoplasms. Endocrine 2022;76:369-376. |
| [89] | Bachelot A, Cailleux AF, Klain M, Baudin E, Ricard M, Bellon N, et al. Relationship between tumor burden and serum thyroglobulin level in patients with papillary and follicular thyroid carcinoma. Thyroid 2022;12:707-711. |
| [90] | Giovanella L, D'Aurizio F, Petranović Ovčariček P, Görges R.Diagnostic, theranostic and prognostic value of thyroglobulin in thyroid cancer. J Clin Med 2024;13:2463. |
| [91] | Xu H, Zhang Y, Wu H, Zhou N, Li X, Pineda JP, et al. High diagnostic accuracy of epigenetic imprinting biomarkers in thyroid nodules. J Clin Oncol 2023;41:1296-1306. |
| [92] | Lee SE, Hwang TS, Choi YL, Kim WY, Han HS, Lim SD, et al. Molecular profiling of papillary thyroid carcinoma in korea with a high prevalence of BRAFV600E mutation. Thyroid 2017;27:802-810. |
| [93] | Marchetti I, Lessi F, Mazzanti CM, Bertacca G, Elisei R, Coscio GD, et al. A morpho-molecular diagnosis of papillary thyroid carcinoma: BRAF V600E detection as an important tool in preoperative evaluation of fine-needle aspirates. Thyroid 2009;19:837-842. |
| [94] | Zhao H, Li H. Meta-analysis of ultrasound for cervical lymph nodes in papillary thyroid cancer: Diagnosis of central and lateral compartment nodal metastases. Eur J Radiol 2019;112:14-21. |
| [95] | Baek HJ, Kim DW, Shin GW, Heo YJ, Baek JW, Lee YJ, et al. Ultrasonographic features of papillary thyroid carcinomas according to their subtypes. Front Endocrinol (Lausanne) 2018;9:223. |
| [96] | Li X, Zhou W, Zhan W.Clinical and ultrasonographic features of medullary thyroid microcarcinomas compared with papillary thyroid microcarcinomas: a retrospective analysis. BMC Med Imaging 2020;20:49. |
| [97] | Radzina M, Ratniece M, Putrins DS, Saule L, Cantisani V.Performance of contrast-enhanced ultrasound in thyroid nodules: review of current state and future perspectives. Cancers (Basel) 2021;13:5469. |
| [98] | Zhang Y, Luo YK, Zhang MB, Li J, Li J, Tang J. Diagnostic accuracy of contrast-enhanced ultrasound enhancement patterns for thyroid nodules. Med Sci Monit 2016;22:4755-4764. |
| [99] | Wu Q, Wang Y, Li Y, Hu B, He ZY. Diagnostic value of contrast-enhanced ultrasound in solid thyroid nodules with and without enhancement. Endocrine 2016;53:480-488. |
| [100] | Wang Y, Dong T, Nie F, Wang G, Liu T, Niu Q.Contrast-enhanced ultrasound in the differential diagnosis and risk stratification of ACR TI-RADS Category 4 and 5 thyroid nodules with non-hypovascular. Front Oncol 2021;11:662273. |
| [1] | Xia ShuJun, Zheng YuHang, Hua Qing, Wei MinYan, Wen Jing, Luo XiaoMao, Yan JiPing, Bai BaoYan, Liu Fang, Dong YiJie, Zhou JianQiao, behalf of The Chinese Artificial Intelligence Alliance for Thyroid on, Ultrasound Breast. Super-Resolution Ultrasound-Based Habitat Imaging: A Consensus Statement [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 97-102. |
| [2] | Zhang Juan, Shen Cuiqin, Du Lianfang, Li Fan. The Application of Ultrasound in the Pre-operative Evaluation of Cervical Cancer [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 163-170. |
| [3] | Liu Jianjun, Zhang Jun, Xue Yafang, Chen Ying, Qiu Mei, Guo Yanli. Ultrasonographic Characteristics and Outcomes of Fetal Umbilical-portal-systemic Venous Shunts: A Single-center Study [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 181-188. |
| [4] | Lin Jiaojiao, Ke Helin, Xu Shaodan, Xiao Yang, Han Lina, Lyu Guorong, Li Shilin. Improved Ultrasound Evaluation Method for Diagnosing Nonalcoholic Fatty Pancreatic Disease: Correlation with MRI mDixon-Quant [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 207-214. |
| [5] | Sun Yang, Li Mofan, Wang Shumin. Tietze Syndrome in A Female POST-COVID-19 Infection: A Review of Current Understanding and Ultrasound Diagnosis [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 215-218. |
| [6] | Liu Xinyu, Yuan Yinuo, Meng Yao, Zhang Wenjing, Xu Huimin, Zhang Jinrui, Liu Cun. Glomus Tumor of the Female Vulva: A Case Report and Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 219-223. |
| [7] | Zhai Yue, Tan Dianhuan, Lin Xiaona, Lv Heng, Chen Yan, Li Yongbin, Luo Haiyu, Dan Qing, Zhao Chenyang, Xiang Hongjin, Zheng Tingting, Sun Desheng. Ultrasound Radiogenomics-based Prediction Models for Gene Mutation Status in Breast Cancer [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 10-20. |
| [8] | Bao Rui, Chen Lu, Luo Yukun, Zhang Mingbo. Advances in the Application of New Ultrasound Technology for the Diagnosis and Treatment of Lymphoma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 32-40. |
| [9] | Zhu Jianing, Li Nan, Luo Yukun, Li Qiuyang. Application of Intraoperative Ultrasound in Robot-assisted Thrombectomy for Renal Cell Carcinoma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 47-49. |
| [10] | Hong Fei, Xu Fei. Application of Low Intensity Ultrasound in the Treatment of Alzheimer’s Disease [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 50-55. |
| [11] | Wang Yixuan, Jin Lin, Chen Jianxiong, Yang Huixian, Shen Cuiqin, Xu Wenzhe, Shen Yuzhou, Huang Jun, Sun Liwan, Du Lianfang, Wang Bei, Li Fan, Li Zhaojun. Is the Adventitial Vasa Vasorum in Vulnerable Carotid Plaques Increased or Decreased? [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 56-64. |
| [12] | Shama Shiti, Xie Xinxin, Wu Ruiqi, He Ping, Li Xiaoda, Chen Qingfeng, Liang Xiaolong. Advancements in BaTiO3-Based Ultrasound‐Triggered Piezoelectric Catalysis for Tumor Therapy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 231-241. |
| [13] | Mohammed Amr, Tahmasebi Aylin, Kim Sooji, Alnoury Mostafa, E. Wessner Corinne, Siu Xiao Tania, W. Gould Sharon, A. May Lauren, Kecskemethy Heidi, T. Saul David, R. Eisenbrey John. Evaluation of Liver Fibrosis on Grayscale Ultrasound in a Pediatric Population Using a Cloud-based Transfer Learning Artificial Intelligence Platform [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 242-249. |
| [14] | Yuzhou Shen, MD, Lin Jin, MD, Lei Sha, MD, Mengmeng Cao, MD, Desheng Sun, MD, Li Liu, MD, Zhaojun Li, MD. Can Different Expertise Levels of Ultrasound Operators Accurately Screen with Handheld Ultrasound? [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(3): 116-123. |
| [15] | Yuhang Zheng, BS, Jianqiao Zhou, MD. Deep Learning in Ultrasound Localization Microscopy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(3): 86-92. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
Share: WeChat
Copyright ©2018 Advanced Ultrasound in Diagnosis and Therapy
|
 Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
