Advanced Ultrasound in Diagnosis and Therapy ›› 2025, Vol. 9 ›› Issue (2): 207-214.doi: 10.37015/AUDT.2025.230059
• Original Research • Previous Articles Next Articles
Lin Jiaojiaoa,b,1, Ke Helina,1, Xu Shaodana, Xiao Yanga, Han Linaa, Lyu Guoronga,c,*( ), Li Shilina,*(
), Li Shilina,*( )
)
Received:2024-01-04
Revised:2023-12-06
Accepted:2024-09-05
Online:2025-06-30
Published:2025-07-06
Contact:
Address Department of Medicine, Quanzhou Medical College. No. 2 Anji Road, Luojiang District, Quanzhou, 362000, China (GRL).e-mail: About author:First author contact:1Jiaojiao Lin and Helin Ke contributed equally to this paper.
Lin Jiaojiao, Ke Helin, Xu Shaodan, Xiao Yang, Han Lina, Lyu Guorong, Li Shilin. Improved Ultrasound Evaluation Method for Diagnosing Nonalcoholic Fatty Pancreatic Disease: Correlation with MRI mDixon-Quant. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 207-214.
Table 1
Improved ultrasonic diagnostic method nonalcoholic fatty pancreatic disease grading standards"
| Grade | Compared with echo of RC | Pancreas itself | Pancreatic duct | Pancreatic outline | SMA、PV |
|---|---|---|---|---|---|
| 0 | No difference | No enlargement | Visible | Smooth | Clearly visible |
| 1 | Mild Enhancement | No enlargement | Visible | Smooth | Clearly visible |
| 2 | Moderate enhancement | Enlargement | Blurred | Blurred | Blurred |
| 3 | Significant enhancement | Significant enlargement | Invisible | Invisible | Invisible |
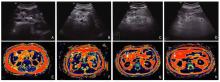
Figure 1
Improved ultrasound grading criteria for Nonalcoholic Fatty Pancreas Disease (NAFPD). (A-D) represent ultrasound images for NAFPD Grades 0 to 3, respectively, with pancreatic tissue (☆), retroperitoneal visceral fat (black arrow), and splenic vein (SV) annotated. (E-H) Corresponding magnetic resonance imaging (MRI) findings of abdominal fat distribution (white arrow) for NAFPD Grades 0-3."
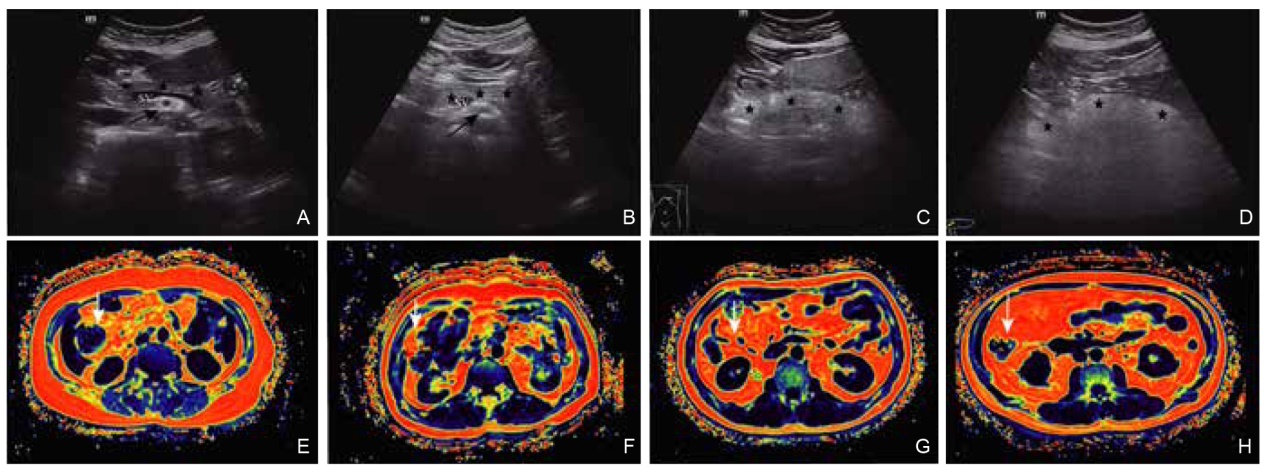
Figure 2
(A) A 54-year-old female US image, with a NAFPD score of grade 1; (B) mDixon-quant image of the same subject as in (A), showing a fat quantification of 0.54%; (C) A 52-year-old female US image, with a NAFPD score of grade 3; (D) mDixon-quant image of the same subject as in (C), showing a fat quantification of 11.84%. Arrow: Pancreas."
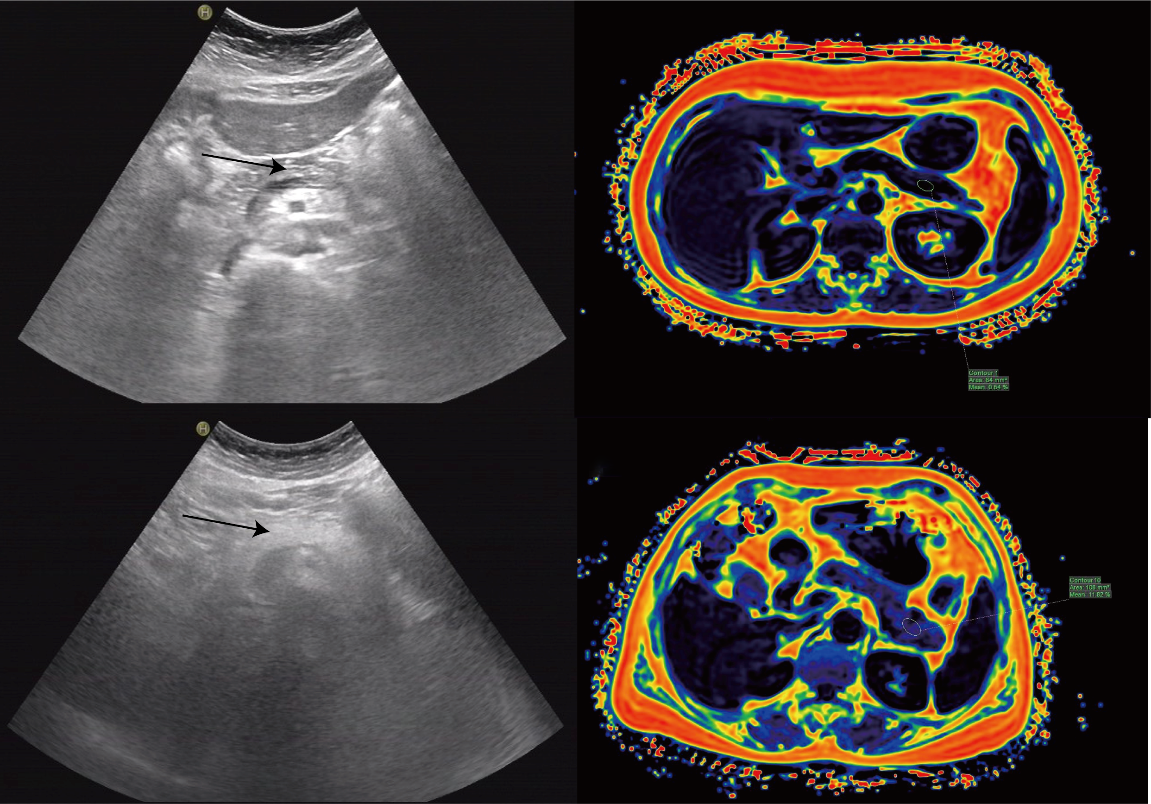

Figure 3
(A) Receiver operating characteristic curve of the traditional version of ultrasound and improved ultrasonic diagnostic method for the diagnosis of nonalcoholic fatty pancreatic disease; (B) and (C) Correlation between pancreatic fat fraction and grade as determined using two pancreatic ultrasound grading methods."
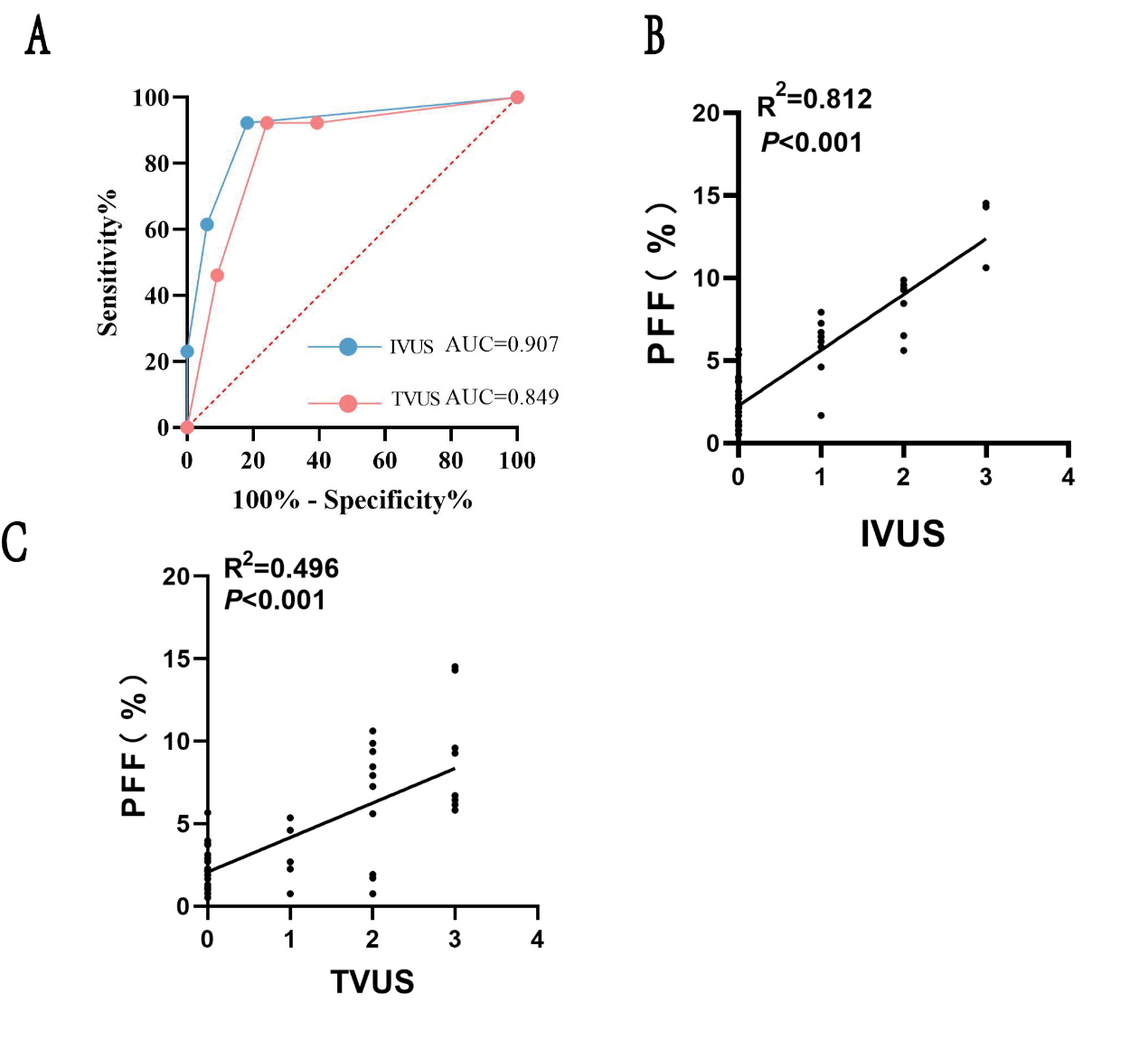
Table 3
Comparison of anthropometric and biochemical parameters of subjects in normal and nonalcoholic fatty pancreatic disease groups and Comparison of visceral fat area and the fat fraction"
| Project | Normal group | NAFPD group | t value | P value |
|---|---|---|---|---|
| Male, cases | 19 (57.6%) | 9 (69.2%) | 0.53 | 0.47 |
| Age, years | 50.77 ± 14.06 | 52.64 ± 12.87 | 0.43 | 0.67 |
| Weight (kg) | 65.67 ± 12.18 | 76.31 ± 12.07 | -2.67 | 0.01 |
| BMI (kg/m2) | 23.93 ± 2.86 | 27.25 ± 2.83 | -3.55 | < 0.01 |
| NAFLD, cases | 12 (38.7%) | 11 (73.3%) | 4.85 | 0.03 |
| TC (mmol/L) | 4.80 ± 0.97 | 4.96 ± 0.41 | -0.52 | 0.61 |
| TG (mmol/L) | 1.42 ± 0.58 | 2.13 ± 1.58 | -2.09 | 0.04 |
| HDL-C (mmol/L) | 1.22 ± 0.28 | 1.10 ± 0.30 | 1.25 | 0.22 |
| LDL-C (mmol/L) | 3.22 ± 0.85 | 3.25 ± 0.57 | -0.09 | 0.99 |
| FPG (mmol/L) | 5.99 ± 1.74 | 6.52 ± 2.37 | -0.78 | 0.43 |
| UA (mmol/L) | 349.50 ± 74.70 | 349.80 ± 93.10 | 0.01 | 0.99 |
| ALT (U/L) | 21.00 (15.00, 36.00) | 27.4 (14.00, 54.50) | -0.80 | 0.42 |
| AST (U/L) | 22.00 (17.00, 32.00) | 26.0 0 (18.50, 30.50) | -0.53 | 0.59 |
| TA (cm2) | 118.80 (95.30, 168.20) | 184.00 (156.40, 26.30) | -3.01 | < 0.01 |
| SA (cm2) | 55.50 (42.80, 78.60) | 61.80 (51.5, 87.60) | -1.45 | 0.15 |
| VA (cm2) | 61.50 (38.90, 91.90) | 117.20 (73.30, 168.90) | -2.89 | < 0.01 |
| VFP (%) | 54.30 ± 12.30 | 62.80 ± 12.90 | -2.08 | 0.04 |
| Subcutaneous fat thickness (cm) | 15.10 (13.3, 20.1) | 17.10 (12.9, 24.9) | -1.14 | 0.25 |
| AC (cm) | 87.15 ± 9.13 | 94.94 ± 5.38 | -2.87 | < 0.01 |
| Pancreatic head fat fraction | 1.86 (1.06, 3.84) | 7.60 (5.91, 11.30) | -4.42 | < 0.01 |
| Pancreatic body fat fraction | 2.63 (0.84, 3.92) | 9.75 (7.39, 13.21) | -5.16 | < 0.01 |
| Pancreatic tail fat fraction | 2.17 (0.95, 3.38) | 10.04 (7.72, 12.44) | -4.89 | < 0.01 |
| PFF | 2.15 (1.12, 3.94) | 9.32 (7.43, 10.43) | -5.23 | < 0.01 |
| HFF | 2.81 (1.78, 5.45) | 8.73 (3.74, 13.50) | -2.54 | 0.01 |
Table 4
Analysis of factors associated with nonalcoholic fatty pancreatic disease"
| Project | r value | P value |
|---|---|---|
| Age | 0.20 | 0.18 |
| Weight | 0.43 | < 0.01 |
| BMI | 0.50 | < 0.01 |
| TC | 0.17 | 0.40 |
| TG | 0.33 | 0.05 |
| HDL-c | -0.07 | 0.69 |
| LDL-c | 0.04 | 0.82 |
| FPG | 0.17 | 0.31 |
| TA | 0.45 | < 0.02 |
| SA | 0.28 | 0.06 |
| VA | 0.45 | < 0.02 |
| VFP | 0.31 | 0.03 |
| AC | 0.48 | < 0.01 |
| HFF | 0.36 | 0.01 |
| [1] | Chen Y, Peng Q, Yang Y, Zheng S, Wang Y, Lu W.The prevalence and increasing trends of overweight, general obesity, and abdominal obesity among chinese adults: A repeated cross-sectional study. BMC Public Health 2019;19:1293. |
| [2] | Lockhart SM, O'Rahilly S.When two pandemics meet: Why is obesity associated with increased COVID-19 mortality? Med (N Y) 2020;1:33-42. |
| [3] | Smits MM, van Geenen EJ. The clinical significance of pancreatic steatosis. Nat Rev Gastroenterol Hepatol 2011;8:169-177. |
| [4] | Ogilvie RF. The islands of langerhans in 19 cases of obesity. J. Pathol 1933;37:473-481 |
| [5] | Dite P, Blaho M, Bojkova M, Jabandziev P, Kunovsky L. Nonalcoholic fatty pancreas disease: Clinical consequences. Dig Dis 2020;38:143-149. |
| [6] | Wagner R, Eckstein SS, Yamazaki H, Gerst F, Machann J, Jaghutriz BA, et al. Metabolic implications of pancreatic fat accumulation. Nature Reviews Endocrinology 2022;18:43-54. |
| [7] | Bi Y, Wang JL, Li ML, Zhou J, Sun XL.The association between pancreas steatosis and metabolic syndrome: A systematic review and meta-analysis. Diabetes Metab Res Rev 2019;35:e3142. |
| [8] | Rahier J, Loozen S, Goebbels RM, Abrahem M. The haemochromatotic human pancreas: A quantitative immunohistochemical and ultrastructural study. Diabetologia 1987;30:5-12. |
| [9] | Rofsky NM, Lee VS, Laub G, Pollack MA, Krinsky GA, Thomasson D, et al. Abdominal MR imaging with a volumetric interpolated breath-hold examination. Radiology 1999;212:876-884. |
| [10] | Zhang Y, Zhou Z, Wang C, Cheng X, Wang L, Duanmu Y, et al. Reliability of measuring the fat content of the lumbar vertebral marrow and paraspinal muscles using MRI mdixon-quant sequence. Diagn Interv Radiol 2018;24:302-307. |
| [11] | Sezgin O, Yaraş S, Özdoğan O. Pancreatic steatosis is associated with both metabolic syndrome and pancreatic stiffness detected by ultrasound elastography. Dig Dis Sci 2022;67:293-304. |
| [12] | Della Corte C, Mosca A, Majo F, Lucidi V, Panera N, Giglioni E, et al. Nonalcoholic fatty pancreas disease and nonalcoholic fatty liver disease: More than ectopic fat. Clin Endocrinol (Oxf) 2015;83:656-662. |
| [13] | Piskin FC, Yavuz S, Kose S, Cagli C, Dogruel D, Tumgor G, et al. A comparative study of the pancreas in pediatric patients with cystic fibrosis and healthy children using two-dimensional shear wave elastography. J Ultrasound 2020;23:535-542. |
| [14] | Smereczyński A, Kołaczyk K.Is a fatty pancreas a banal lesion? Journal of ultrasonography 2016;16:273-280. |
| [15] | Singh RG, Yoon HD, Wu LM, Lu J, Plank LD, Petrov MS. Ectopic fat accumulation in the pancreas and its clinical relevance: A systematic review, meta-analysis, and meta-regression. Metabolism 2017;69:1-13. |
| [16] | Ferraioli G, Monteiro LBS. Ultrasound-based techniques for the diagnosis of liver steatosis. World J Gastroenterol 2019;25:6053-6062. |
| [17] | Johnson ML, Mack LA. Ultrasonic evaluation of the pancreas. Gastrointest Radiol 1978;3:257-266. |
| [18] | Tong X, Dai C, Walker JT, Nair GG, Kennedy A, Carr RM, et al. Lipid droplet accumulation in human pancreatic islets is dependent on both donor age and health. Diabetes 2020;69:342-354. |
| [19] | Rugivarodom M, Geeratragool T, Pausawasdi N, Charatcharoenwitthaya P. Fatty pancreas: Linking pancreas pathophysiology to nonalcoholic fatty liver disease. Journal of clinical and translational hepatology. 2022;10:1229-1239 |
| [20] | Ramkissoon R, Gardner TB. Pancreatic steatosis: An update. Curr Opin Gastroenterol 2019;35:440-447. |
| [21] | Yamazaki H, Tauchi S, Kimachi M, Dohke M, Hanawa N, Kodama Y, et al. Independent association between prediabetes and future pancreatic fat accumulation: A 5-year japanese cohort study. Journal of gastroenterology 2018;53:873-882. |
| [22] | Ramkissoon R, Gardner TB. Pancreatic steatosis: An emerging clinical entity. Am J Gastroenterol 2019;114:1726-1734. |
| [23] | Longo M, Zatterale F, Naderi J, Parrillo L, Formisano P, Raciti GA, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci 2019;20. |
| [24] | Hansen JB, Dos Santos LRB, Liu Y, Prentice KJ, Teudt F, Tonnesen M, et al. Glucolipotoxic conditions induce β-cell iron import, cytosolic ros formation and apoptosis. J Mol Endocrinol 2018;61:69-77. |
| [25] | Wang X, Misawa R, Zielinski MC, Cowen P, Jo J, Periwal V, et al. Regional differences in islet distribution in the human pancreas--preferential beta-cell loss in the head region in patients with type 2 diabetes PLoS One 2013;8:e67454. |
| [26] | Pfeifer CD, Schoennagel BP, Grosse R, Wang ZJ, Graessner J, Nielsen P, et al. Pancreatic iron and fat assessment by mri-r2* in patients with iron overload diseases. Journal of Magnetic Resonance Imaging 2015;42:196-203. |
| [27] | Gerst F, Wagner R, Oquendo MB, Siegel-Axel D, Fritsche A, Heni M, et al. What role do fat cells play in pancreatic tissue? Mol Metab 2019;25:1-10. |
| [28] | Ranasinghe P, Mathangasinghe Y, Jayawardena R, Hills AP, Misra A.Prevalence and trends of metabolic syndrome among adults in the asia-pacific region: A systematic review. BMC Public Health 2017;17:101. |
| [29] | Ansarimoghaddam A, Adineh HA, Zareban I, Iranpour S, HosseinZadeh A, Kh F. Prevalence of metabolic syndrome in middle-east countries: Meta-analysis of cross-sectional studies. Diabetes Metab Syndr 2018;12:195-201. |
| [30] | Zhou J, Li ML, Zhang DD, Lin HY, Dai XH, Sun XL, et al. The correlation between pancreatic steatosis and metabolic syndrome in a Chinese population. Pancreatology 2016;16:578-583. |
| [1] | Xia ShuJun, Zheng YuHang, Hua Qing, Wei MinYan, Wen Jing, Luo XiaoMao, Yan JiPing, Bai BaoYan, Liu Fang, Dong YiJie, Zhou JianQiao, behalf of The Chinese Artificial Intelligence Alliance for Thyroid on, Ultrasound Breast. Super-Resolution Ultrasound-Based Habitat Imaging: A Consensus Statement [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 97-102. |
| [2] | Ye Beibei, Zhang Yifeng. Preoperative Diagnosis of Thyroid Follicular Tumor [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 127-137. |
| [3] | Zhang Juan, Shen Cuiqin, Du Lianfang, Li Fan. The Application of Ultrasound in the Pre-operative Evaluation of Cervical Cancer [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 163-170. |
| [4] | Liu Jianjun, Zhang Jun, Xue Yafang, Chen Ying, Qiu Mei, Guo Yanli. Ultrasonographic Characteristics and Outcomes of Fetal Umbilical-portal-systemic Venous Shunts: A Single-center Study [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 181-188. |
| [5] | Sun Yang, Li Mofan, Wang Shumin. Tietze Syndrome in A Female POST-COVID-19 Infection: A Review of Current Understanding and Ultrasound Diagnosis [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 215-218. |
| [6] | Liu Xinyu, Yuan Yinuo, Meng Yao, Zhang Wenjing, Xu Huimin, Zhang Jinrui, Liu Cun. Glomus Tumor of the Female Vulva: A Case Report and Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 219-223. |
| [7] | Zhai Yue, Tan Dianhuan, Lin Xiaona, Lv Heng, Chen Yan, Li Yongbin, Luo Haiyu, Dan Qing, Zhao Chenyang, Xiang Hongjin, Zheng Tingting, Sun Desheng. Ultrasound Radiogenomics-based Prediction Models for Gene Mutation Status in Breast Cancer [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 10-20. |
| [8] | Bao Rui, Chen Lu, Luo Yukun, Zhang Mingbo. Advances in the Application of New Ultrasound Technology for the Diagnosis and Treatment of Lymphoma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 32-40. |
| [9] | Zhu Jianing, Li Nan, Luo Yukun, Li Qiuyang. Application of Intraoperative Ultrasound in Robot-assisted Thrombectomy for Renal Cell Carcinoma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 47-49. |
| [10] | Hong Fei, Xu Fei. Application of Low Intensity Ultrasound in the Treatment of Alzheimer’s Disease [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 50-55. |
| [11] | Wang Yixuan, Jin Lin, Chen Jianxiong, Yang Huixian, Shen Cuiqin, Xu Wenzhe, Shen Yuzhou, Huang Jun, Sun Liwan, Du Lianfang, Wang Bei, Li Fan, Li Zhaojun. Is the Adventitial Vasa Vasorum in Vulnerable Carotid Plaques Increased or Decreased? [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 56-64. |
| [12] | Shama Shiti, Xie Xinxin, Wu Ruiqi, He Ping, Li Xiaoda, Chen Qingfeng, Liang Xiaolong. Advancements in BaTiO3-Based Ultrasound‐Triggered Piezoelectric Catalysis for Tumor Therapy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 231-241. |
| [13] | Mohammed Amr, Tahmasebi Aylin, Kim Sooji, Alnoury Mostafa, E. Wessner Corinne, Siu Xiao Tania, W. Gould Sharon, A. May Lauren, Kecskemethy Heidi, T. Saul David, R. Eisenbrey John. Evaluation of Liver Fibrosis on Grayscale Ultrasound in a Pediatric Population Using a Cloud-based Transfer Learning Artificial Intelligence Platform [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(4): 242-249. |
| [14] | Yuzhou Shen, MD, Lin Jin, MD, Lei Sha, MD, Mengmeng Cao, MD, Desheng Sun, MD, Li Liu, MD, Zhaojun Li, MD. Can Different Expertise Levels of Ultrasound Operators Accurately Screen with Handheld Ultrasound? [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(3): 116-123. |
| [15] | Yuhang Zheng, BS, Jianqiao Zhou, MD. Deep Learning in Ultrasound Localization Microscopy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2024, 8(3): 86-92. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
Share: WeChat
Copyright ©2018 Advanced Ultrasound in Diagnosis and Therapy
|
 Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
