Advanced Ultrasound in Diagnosis and Therapy ›› 2025, Vol. 9 ›› Issue (1): 56-64.doi: 10.37015/AUDT.2025.240043
• Original Research • Previous Articles Next Articles
Wang Yixuana,b,1, Jin Linc,1, Chen Jianxionga,d, Yang Huixiane, Shen Cuiqina, Xu Wenzhea, Shen Yuzhoua, Huang Juna, Sun Liwana, Du Lianfangf, Wang Beib, Li Fanf, Li Zhaojuna,f,*( )
)
Received:2024-08-18
Revised:2024-09-08
Accepted:2024-10-24
Online:2025-03-30
Published:2025-02-08
Contact:
Department of Ultrasound, Jiading Branch of Shanghai General Hospital, Shanghai Jiaotong University School of Medicine, 800 Huangjiahuayuan Road, Jiading District, Shanghai, 201803, China e-mail: About author:First author contact:1 Yixuan Wang and Lin Jin contributed equally to this study.
Wang Yixuan, Jin Lin, Chen Jianxiong, Yang Huixian, Shen Cuiqin, Xu Wenzhe, Shen Yuzhou, Huang Jun, Sun Liwan, Du Lianfang, Wang Bei, Li Fan, Li Zhaojun. Is the Adventitial Vasa Vasorum in Vulnerable Carotid Plaques Increased or Decreased?. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 56-64.
Table 1
Demographic details and US characteristics of the 47 participants"
| Item | Without cerebral infarction (n = 19) | With cerebral infarction (n = 28) | t/ꭓ2 | P value |
|---|---|---|---|---|
| Gender(F/M) | 7/12 | 5/23 | 1.263 | 0.261 |
| Age, y | 64.37 ± 6.66 | 67.43 ± 7.90 | -1.385 | 0.173 |
| Height, cm | 166.66 ± 8.12 | 170.30 ± 6.85 | -1.660 | 0.104 |
| Weight, kg | 62.90 ± 9.11 | 67.13 ± 9.64 | -1.511 | 0.138 |
| BMI | 22.63 ± 2.80 | 23.04 ± 2.31 | -5.45 | 0.588 |
| SBP, mm Hg | 144.05 ± 14.52 | 143.25 ± 19.72 | 0.152 | 0.880 |
| DBP, mm Hg | 90.11 ± 8.82 | 89.54 ± 11.81 | 0.179 | 0.859 |
| PP, mm Hg | 53.95 ± 6.61 | 53.71 ± 9.38 | 0.094 | 0.926 |
| Hypertension(with/without)* | 6/11 | 11/13 | 0.455 | 0.500 |
| Diabetes(with/without)※ | 5/12 | 8/16 | 0.071 | 0.790 |
| US characteristics | ||||
| Plaque thickness, mm | 3.07 ± 1.03 | 3.28 ± 1.15 | -0.645 | 0.522 |
| Plaque length, mm | 11.39 ± 5.72 | 11.17 ± 5.01 | 0.141 | 0.889 |
| Plaque echogenicity | 1.070 | 1.000 | ||
| Hypoechoic | 7 | 11 | ||
| Isoechoic | 0 | 1 | ||
| Hyperechoic | 1 | 1 | ||
| Mixed echogenicity | 11 | 15 | ||
| CEUS characteristics | ||||
| ROIplaque | -41.75 ± 6.11 | -43.09 ± 10.35 | 0.556 | 0.581 |
| ROI | -39.00 ± 6.50 | -38.83 ± 8.76 | -0.075 | 0.940 |
Table 2
Demographic Details of the 21 Patients"
| Number | Gender(F/M) | Age (y) | The length of plaque (mm) | The width of plaque (mm) | The location of plaque | Cerebral infarction (Yes/No) |
|---|---|---|---|---|---|---|
| 1 | M | 72 | 27.40 | 5.8 | RICA | Yes |
| 2 | M | 83 | 20.30 | 5.2 | LICA | Yes |
| 3 | M | 80 | 27.80 | 5.7 | RICA | Yes |
| 4 | M | 71 | 19.70 | 5.4 | LICA | Yes |
| 5 | M | 69 | 14.30 | 5.6 | LICA | NO |
| 6 | M | 60 | 23.90 | 6.1 | RICA | Yes |
| 7 | M | 64 | 26.30 | 4.6 | RICA | Yes |
| 8 | M | 63 | 6.79 | 4.07 | LICA | Yes |
| 9 | F | 72 | 23.20 | 5.1 | LICA | Yes |
| 10 | M | 65 | 14.50 | 4.1 | LICA | Yes |
| 11 | M | 55 | 28.30 | 4.9 | LICA | NO |
| 12 | M | 74 | 14.60 | 5.3 | LECA | Yes |
| 13 | F | 89 | 18.70 | 5.5 | RICA | Yes |
| 14 | M | 86 | 12.40 | 3.6 | RICA | Yes |
| 15 | M | 64 | 26.30 | 5.1 | LICA | Yes |
| 16 | M | 66 | 22.70 | 5.7 | RICA | Yes |
| 17 | M | 59 | 20.90 | 5.6 | RICA | Yes |
| 18 | M | 70 | 33.50 | 4.6 | LICA | NO |
| 19 | M | 82 | 8.20 | 4.3 | RICA | Yes |
| 20 | M | 78 | 19.30 | 4.8 | LICA | Yes |
| 21 | M | 62 | 17.10 | 5.4 | RICA | Yes |
Table 3
Comparison of CT values of different locations of carotid artery"
| Imaging modality | CT value of vascular wall behind the dominant plaque | CT value of ipsilateral wall of dominant plaque | CT value of contralateral wall of dominant plaque | CT value of adjacent wall of dominant plaque | CT value of shoulder of plaque | CT value of bottom of plaque | CT value of center of plaque |
|---|---|---|---|---|---|---|---|
| CT plain scan | 44.68 ± 8.02 | 50.42 ± 7.63 | 51.71 ± 7.93 | 50.42 ± 7.63 | 38.78 ± 7.43 | 38.08 ± 6.33 | 26.30 ± 8.43 |
| Enhanced CT scan | 43.48 ± 10.15* | 71 ± 17.65 | 82.31 ± 21.34 | 71.00 ± 17.65 | 64.33 ± 12.33 | 46.75 ± 10.86 | 32.40 ± 9.71 |
| T value | 0.425 | -4.905 | -6.186 | -4.905 | -8.138 | -3.161 | -2.173 |
| P value | 0.673 | <0.001 | <0.001 | <0.001 | <0.001 | 0.003 | 0.036 |

Figure 5
CEUS and CTA images. (A) Images of a 61-year-old man with plaque at carotid artery bifurcation. ① CT value of the inside of plaque was 36.1 HU. CT value of vascular wall behind the dominant plaque (51.5 HU) was lower than ipsilateral wall of dominant plaque (93.5 HU). ② Image of three-dimensional reconstruction of this patient and the arrow indicated the location of carotid plaque. ③ Peak intensity of the inside of plaque was 0 dB. Peak intensity of vascular wall behind the dominant plaque (1.98 dB) was lower than ipsilateral wall of dominant plaque (4.67 dB). (B) Images of a 66-year-old man with plaque at carotid artery bifurcation. ① CT value of the inside of plaque was 44.67 HU. CT value of vascular wall behind the dominant plaque (30 HU) was lower than ipsilateral wall of dominant plaque (35 HU). ② Image of three-dimensional reconstruction of this patient and the arrow indicated the location of carotid plaque. ③ Peak intensity of the inside of plaque was 0 dB. Peak intensity of vascular wall behind the dominant plaque (1.36 dB) was lower than ipsilateral wall of dominant plaque (5.44 dB). (C) Images of a 65-year-old man with plaque at carotid artery bifurcation. ① CT value of the inside of plaque was 47.33 HU. CT value of vascular wall behind the dominant plaque (63 HU) was lower than ipsilateral wall of dominant plaque (108 HU). ② Image of three-dimensional reconstruction of this patient and the arrow indicated the location of carotid plaque. ③ Peak intensity of the inside of plaque was 0 dB. Peak intensity of vascular wall behind the dominant plaque (18.98 dB) was lower than ipsilateral wall of dominant plaque (42.32 dB). ABC"
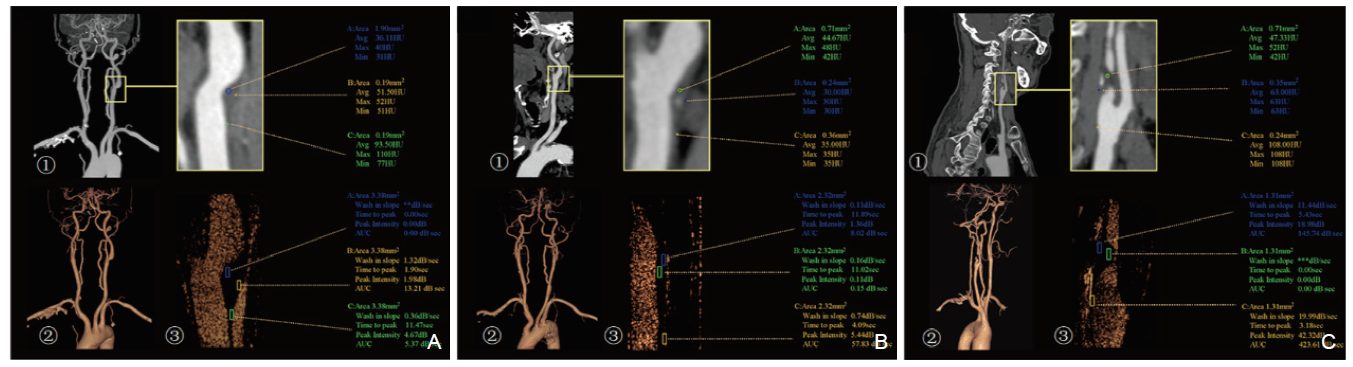
Table 4
Comparison of increased intensity among different locations and thicknesses of tubes"
| ROI | Wall thickness | Concentration | Z value | P value | ||
|---|---|---|---|---|---|---|
| 0.05% | 0.30% | 0.5% | ||||
| ROInear-wall | 2 mm | 0.77 (-1.10,1.28) | -0.73 (0.94,0.38) | 0.01 (-0.32,0.47) | 3.796 | 0.15 |
| 3 mm | 0.28 (0.05,0.98) | 0.17 (-0.06,0.31) | 0.04 (-0.05,0.19) | 2.023 | 0.364 | |
| ROIlumen | 2 mm | 6.51 (6.35,7.50) | 14.05 (13.69,14.29)* | 16.92 (16.44,17.29)*※ | 25.806 | < 0.001 |
| 3 mm | 6.07 (5.84,6.37)ф | 12.70 (12.51,13.14)*ф | 14.82 (14.43,15.05)*ф | 23.484 | < 0.001 | |
| ROIfar-wall | 2 mm | 0.44 (-0.12,0.60) | 3.42 (1.84,8.97)* | 9.02 (6.35,12.78)* | 20.999 | < 0.001 |
| 3 mm | 0.90 (0.34,2.14)ф | 2.68 (2.19,3.49) | 11.02 (9.51,12.72)*※ | 21.835 | < 0.001 | |

Figure 6
CEUS study in vitro with different wall thickness and microbubble concentration. Images of time and intensity curves with contrast agent concentration of 0.05% (A) 2 mm-thickness; (B) 3 mm-thicked tube), 0.3% (C) 2 mm-thickness tube; (D) 3 mm-thickness tube), 0.5% (E) 2 mm-thickness tube; (F) 3 mm-thicknEss tube) show increased intensity of far wall artifact."
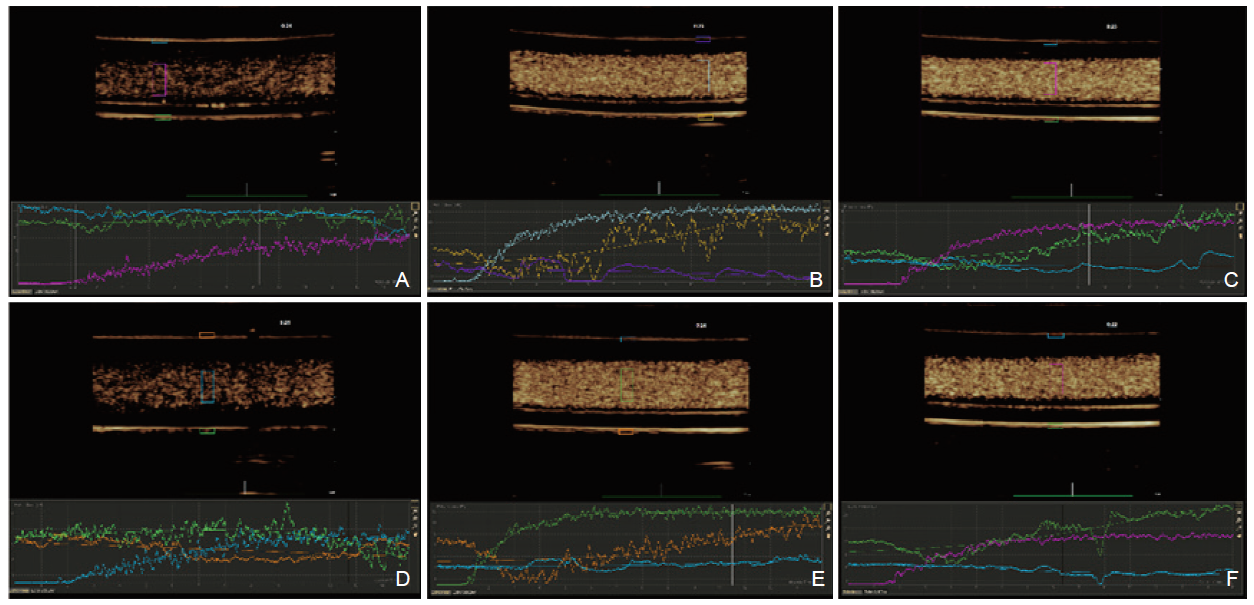
Table 5
Association between increased intensity of different ROI"
| Item | ROInear-wall | ROIlumen | ROIfar-wall |
|---|---|---|---|
| ROInear-wall | r =1.000 | r = -0.231 | r = 0.221 |
| - | P = 0.075 | P = 0.090 | |
| ROIlumen | r = -0.231 | r =1.000 | r = 0.775 |
| P = 0.075 | - | P < 0.001 | |
| ROIfar-wall | r = 0.221 | r = 0.775 | r = 1.000 |
| P = 0.090 | P < 0.001 | - |
Table 6
Associations between increased intensity of ROIfar-wall and ROInear-wall, ROIlumen"
| Model | Unstandardized Coefficients B | Standardized Coefficients Beta | B 95% CI | T value | P value | |
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| (Constant) | -4.683 | -7.444 | -1.922 | -3.397 | 0.001 | |
| ROInear-wall | -0.169 | -0.024 | -1.515 | 1.176 | -0.252 | 0.802 |
| ROIlumen | 0.805 | 0.709 | 0.588 | 1.023 | 7.415 | < 0.001 |
| [1] | Campbell BCV, Khatri P. Stroke. Lancet (London, England) 2020;396:129-142. |
| [2] | Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;394:1145-1158. |
| [3] | Heistad DD, Marcus ML, Larsen GE, Armstrong ML. Role of vasa vasorum in nourishment of the aortic wall. Am J Physiol 1981;240:H781-787. |
| [4] | Subbotin VM. Excessive intimal hyperplasia in human coronary arteries before intimal lipid depositions is the initiation of coronary atherosclerosis and constitutes a therapeutic target. Drug Discov Today 2016;21:1578-1595. |
| [5] | Li Z, Bai Y, Li W, Gao F, Kuang Y, Du L, et al. Carotid vulnerable plaques are associated with circulating leukocytes in acute ischemic stroke patients: an clinical study based on contrast-enhanced ultrasound. Sci Rep 2018;8:8849. |
| [6] | Staub D, Partovi S, Schinkel AF, Coll B, Uthoff H, Aschwanden M, et al. Correlation of carotid artery atherosclerotic lesion echogenicity and severity at standard US with intraplaque neovascularization detected at contrast-enhanced US. Radiology 2011;258:618-626. |
| [7] | Sluimer JC, Gasc JM, van Wanroij JL, Kisters N, Groeneweg M, Sollewijn Gelpke MD, et al. Hypoxia, hypoxia-inducible transcription factor, and macrophages in human atherosclerotic plaques are correlated with intraplaque angiogenesis. J Am Coll Cardiol 2008;51:1258-1265. |
| [8] | Wu X, Reboll MR, Korf-Klingebiel M, Wollert KC. Angiogenesis after acute myocardial infarction. Cardiovasc Res 2021;117:1257-1273. |
| [9] | Thapar A, Shalhoub J, Averkiou M, Mannaris C, Davies AH, Leen EL. Dose-dependent artifact in the far wall of the carotid artery at dynamic contrast-enhanced US. Radiology 2012;262:672-679. |
| [10] | Saba L, Cau R, Murgia A, Nicolaides AN, Wintermark M, Castillo M, et al. Carotid plaque-RADS: A novel stroke risk classification system. JACC Cardiovasc Imaging 2024;17:62-75. |
| [11] | Boyle EC, Sedding DG, Haverich A. Targeting vasa vasorum dysfunction to prevent atherosclerosis. Vascular pharmacology 2017;96-98:5-10. |
| [12] | Sedding DG, Boyle EC, Demandt JAF, Sluimer JC, Dutzmann J, Haverich A, et al. Vasa vasorum angiogenesis: Key player in the initiation and progression of atherosclerosis and potential target for the treatment of cardiovascular disease. Front Immunol 2018;9:706. |
| [13] | Jorgensen SM, Korinek MJ, Vercnocke AJ, Anderson JL, Halaweish A, Leng S, et al. Arterial wall perfusion measured with photon counting spectral X-ray CT. Proc SPIE Int Soc Opt Eng 2016;9967. |
| [14] | Zheng L, Yang WJ, Niu CB, Zhao HL, Wong KS, Leung TWH, et al. Correlation of adventitial vasa vasorum with intracranial atherosclerosis: A postmortem study. Journal of stroke 2018;20:342-349. |
| [15] | Ito H, Wakatsuki T, Yamaguchi K, Fukuda D, Kawabata Y, Matsuura T, et al. Atherosclerotic coronary plaque is associated with adventitial vasa vasorum and local inflammation in adjacent epicardial adipose tissue in fresh cadavers. Circ J 2020;84:769-775. |
| [16] | Sano M, Sasaki T, Baba S, Inuzuka K, Katahashi K, Kayama T, et al. Differences in vasa vasorum distribution in human aortic aneurysms and atheromas. Angiology 2022;73:546-556. |
| [17] | Chistiakov DA, Melnichenko AA, Myasoedova VA, Grechko AV, Orekhov AN. Role of lipids and intraplaque hypoxia in the formation of neovascularization in atherosclerosis. Ann Med 2017;49:661-677. |
| [18] | Ritman EL, Lerman A. The dynamic vasa vasorum. Cardiovasc Res 2007;75:649-658. |
| [19] | Tesfamariam B. Periadventitial local drug delivery to target restenosis. Vascul Pharmacol 2017:S1537- 1891(17)30235-5. |
| [20] | Schinkel AFL, Bosch JG, Staub D, Adam D, Feinstein SB. Contrast-enhanced ultrasound to assess carotid intraplaque neovascularization. Ultrasound Med Biol 2020;46:466-478. |
| [21] | Magnoni M, Coli S, Marrocco-Trischitta MM, Melisurgo G, De Dominicis D, Cianflone D, et al. Contrast-enhanced ultrasound imaging of periadventitial vasa vasorum in human carotid arteries. Eur J Echocardiogr 2009;10:260-264. |
| [22] | Staub D, Patel MB, Tibrewala A, Ludden D, Johnson M, Espinosa P, et al. Vasa vasorum and plaque neovascularization on contrast-enhanced carotid ultrasound imaging correlates with cardiovascular disease and past cardiovascular events. Stroke 2010;41:41-47. |
| [23] | ten Kate GL, Renaud GG, Akkus Z, van den Oord SC, ten Cate FJ, Shamdasani V, et al. Far-wall pseudoenhancement during contrast-enhanced ultrasound of the carotid arteries: clinical description and in vitro reproduction. Ultrasound Med Biol 2012;38:593-600. |
| [1] | Osama Mahmoud, BS, Ajay Makkena, BS, Corinne E. Wessner, MS, MBA, RDMS, Ji-Bin Liu, MD, John R. Eisenbrey, PhD, Andrej Lyshchik, MD, PhD. Contrast-Enhanced Ultrasound LI-RADS: A Pictorial Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(4): 321-332. |
| [2] | Priscilla Machado, MD, Ji-Bin Liu, MD, Flemming Forsberg, PhD. Sentinel Lymph Node Identification Using Contrast Lymphosonography: A Systematic Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(1): 1-7. |
| [3] | Ping Wang, MM, Yuqun Luo, MM, Yunkai Li, MM, Wensheng Yue, MD, Duo Huang, MD, Xuemei Lin, MM, Shaoli Xie, MM, Bin Xiong, MM. A Misdiagnosed Cervical Vagal Schwannoma: A Case Report and Review of Its Imaging Features and Differential Diagnosis [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(1): 53-56. |
| [4] | Felipe Velasquez-Botero, MD, Ananya Balasubramanya, Ying Tang, MD, Qiang Lu, MD, Ji-Bin Liu, MD, John R. Eisenbrey, PhD. Renal Contrast-enhanced Ultrasound: Clinical Applications and Emerging Research [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(4): 129-146. |
| [5] | Yanling Chen, MM, Hantao Wang, MM, Hong Han, PhD, Yi Dong, PhD, Wen-ping Wang, MD. Contrast-enhanced Ultrasound of Undifferentiated Embryonal Sarcoma of the Liver in Adult: Two Cases Report and Literature Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(4): 204-209. |
| [6] | Huolin Ye, MD, Qiannan Huang, MD, Qingjing Zeng, MD, Xuqi He, MD, Erjiao Xu, MD, Yinglin Long, MD, Kai Li, MD, Rongqin Zheng, MD. Contrast-enhanced Ultrasound for Evaluation of Active Needle Tract Bleeding during Thermal Ablation of Liver Cancer [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(3): 104-111. |
| [7] | Xuehong Diao, MD, Lin Chen, MD, Bo Yu, MS, Jiamei Jin, MS, Jia Zhan, MD, Yue Chen, BS. Follicular Thyroid Neoplasmon Conventional and Contrast-enhanced Ultrasound [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(2): 48-57. |
| [8] | Brenda E. Tester, BS, MS, Ji-Bin Liu, MD, John R. Eisenbrey, PhD, George Koenig, MD. Emerging Applications of Contrast-enhanced Ultrasound in Trauma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(2): 39-47. |
| [9] | Tong Zhang, MD, Xiaolin Yin, Shuang Zheng, MD, Mingwei Sui, MD, Dezhi Zhang, MD. Application Value of Two-Dimensional Ultrasound Combined with Contrast-Enhanced Ultrasound for the Diagnosis of Multiple Bile Duct Hamartomas: A Case Report [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(4): 317-320. |
| [10] | Esika Savsani, Mohamed Tantawi, MD, Corinne E. Wessner, MBA, RDMS, RVT, Philip Lee, MD, Andrej Lyshchik, MD, PhD, Kevin Anton, MD, PhD, Colette M. Shaw, MD, Ji-Bin Liu, MD, John R. Eisenbrey, PhD. Contrast-enhanced Ultrasound Assessment of Treatment Response in a Patient with Multifocal Hepatocellular Carcinoma Treated with Transarterial Chemo and Radioembolization [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(3): 254-257. |
| [11] | Danni He, MS, Qiao Ji, MD, Huitong Lin, MD, Xuankun Liang, MM, Lujing Li, MM, Fengping Liang, MM, Xianxiang Wang, MM, Kun Yuan, MS, Zuofeng Xu, MD. A New-Designed Microwave Ablation System: Testing in ex vivo and in vivo Liver Model [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(1): 39-46. |
| [12] | Qiuyang Li, MD, Ying Zhang, MD, Yong Song, MD, Aitao Guo, MD, Nan Li, BS, Yukun Luo, MD, Jie Tang, MD. Clinical Application of Ultrasound in the Diagnosis and Treatment of Reninoma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(3): 211-216. |
| [13] | Mohamed Tantawi, MD, Ji-Bin Liu, MD, John R Eisenbrey, PhD. Recent Advances in Microbubble-Augmented Cancer Therapy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(3): 155-168. |
| [14] | Li Ma, MD, Wenzhao Liang, MD, Yupeng Zhu, MD, Yingqiao Zhu, MD, Dezhi Zhang, MD. Differences in CEUS and CE-MRI Appearance of HCC: A Case Report [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(4): 197-199. |
| [15] | Qing Zhang, MD, Shuping Wei, MD, Bin Yang, MD, Xiaoqin Qian, MD. Differences Between Type I and Type II Papillary Renal Cell Carcinoma on Ultrasound [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(4): 187-192. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
Share: WeChat
Copyright ©2018 Advanced Ultrasound in Diagnosis and Therapy
|
 Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
