Advanced Ultrasound in Diagnosis and Therapy ›› 2022, Vol. 6 ›› Issue (4): 129-146.doi: 10.37015/AUDT.2022.220036
• Review Articles • Previous Articles Next Articles
Felipe Velasquez-Botero, MDa, Ananya Balasubramanyaa, Ying Tang, MDb, Qiang Lu, MDc, Ji-Bin Liu, MDa, John R. Eisenbrey, PhDa,*( )
)
Received:2022-09-14
Revised:2022-10-05
Accepted:2022-10-14
Online:2022-12-30
Published:2022-10-25
Contact:
John R. Eisenbrey, PhD,
E-mail:john.eisenbrey@jefferson.edu
Felipe Velasquez-Botero, MD, Ananya Balasubramanya, Ying Tang, MD, Qiang Lu, MD, Ji-Bin Liu, MD, John R. Eisenbrey, PhD. Renal Contrast-enhanced Ultrasound: Clinical Applications and Emerging Research. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(4): 129-146.
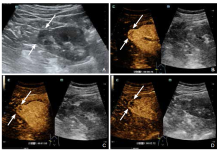
Figure 1
In a 63-year-old male, a hypoechoic nodule measuring 1.8 × 1.8 cm was observed in the lower pole of the right kidney, with an unclear boundary and regular shape that extended outside the kidney (A). An intravenous injection of the ultrasound contrast agent SonoVue resulted in heterogeneous hyperenhancement in the cortical phase (B), isoenhancement in the medullary phase (C), and heterogeneous hypoenhancement in the delayed phase (D) within the nodule. The pathology report confirmed an oncocytoma."
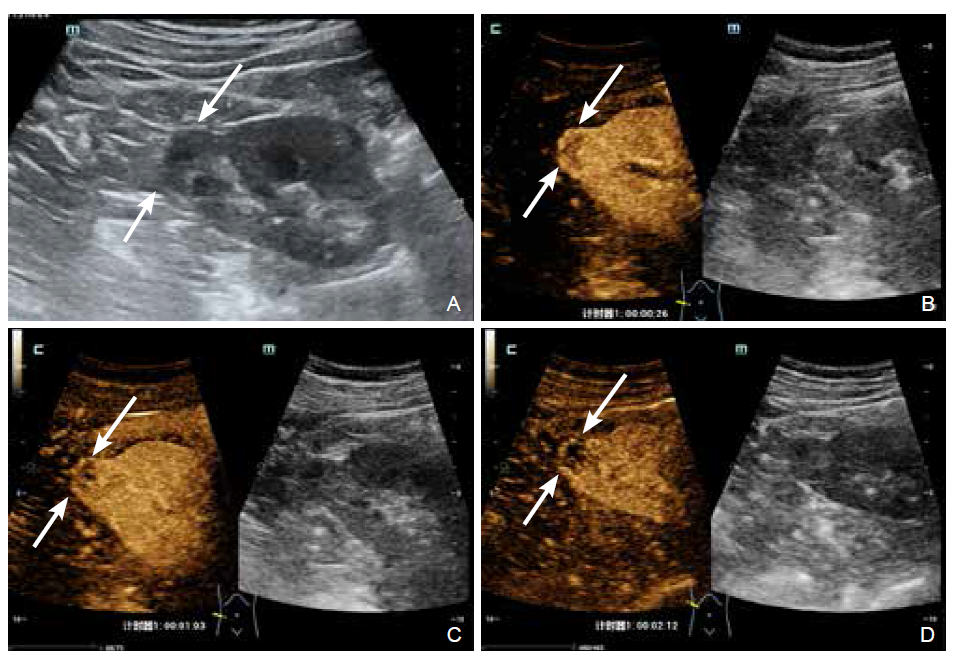

Figure 2
In a 54-year-old male, a 3.0 × 2.4 cm slightly echogenic nodule was seen in the left kidney, with a clear boundary, irregular shape, and extension beyond the renal capsule. After intravenous injection of the ultrasound contrast agent SonoVue, the nodule showed hyperenhancement in cortical phase (A), isoenhancement in medullary phase (B), and slight hypoenhancement in the delayed phase (C). There were small non-enhanced areas seen in all phases. The pathology report confirmed a renal clear cell carcinoma."
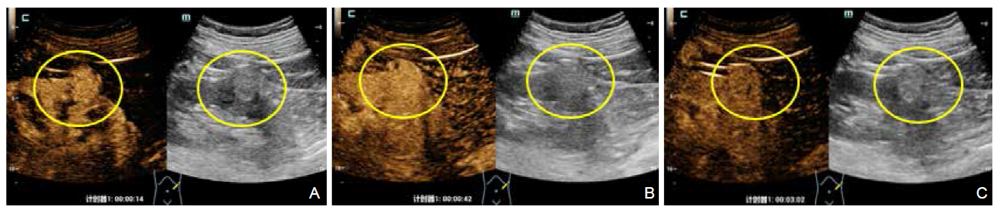
Figure 3
In a 40-year-old female, an echogenic nodule measuring 1.7 × 1.4 cm was detected in the left kidney, with a clear boundary and regular shape. After intravenous injection of the ultrasound contrast agent SonoVue, the nodule demonstrated slightly hyperenhancement in the cortical phase (A) and medullary phase (B). The delayed phase (C) showed isoenhancement. The pathology report confirmed a chromophobe renal carcinoma."
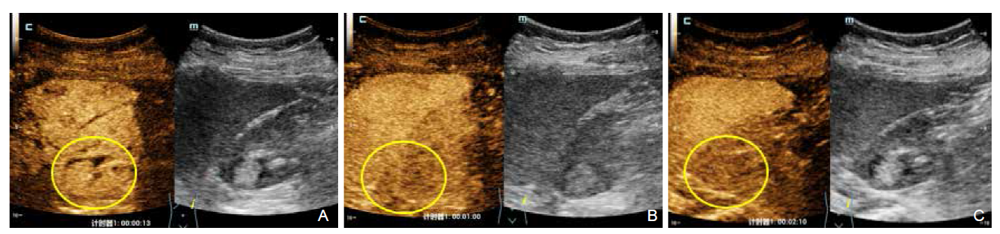

Figure 4
Example of CEUS in the diagnosis of an indeterminate renal mass. (A) Prior to contrast arrival a 7 cm mass (white arrows) is apparent in the right kidney with echoic components on B-mode suggesting solid components and possible malignancy. (B) Following arrival of the contrast agent (2 ml of Lumason, Bracco), no enhancement is observed within the suspected mass (white arrows), indicating it is a hemorrhagic cyst and ruling out RCC."
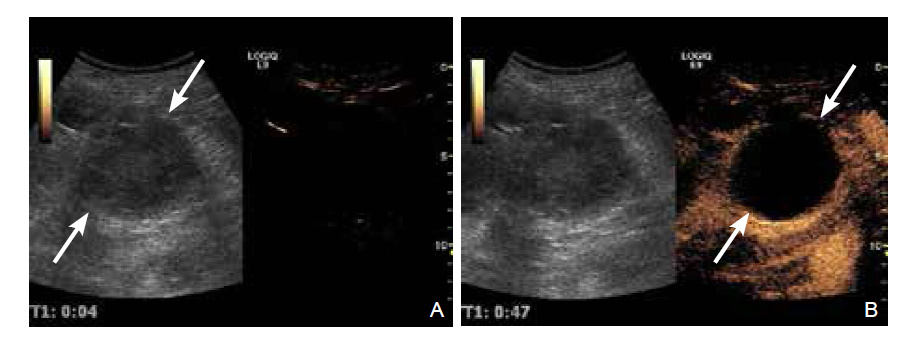
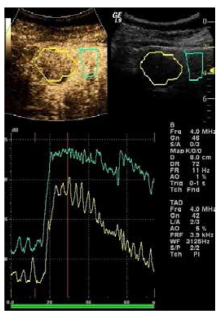
Figure 5
Example CEUS and time-intensity curve analysis of a renal mass later confirmed as papillary RCC on tissue sampling. Top images: Regions of interest are placed around the indeterminate mass (yellow) and adjacent renal cortex (blue). Bottom image: Contrast signal intensity is then plotted as a function of time for each region of interest. Notice the RCC demonstrates faster contrast signal washout relative to the renal parenchyma, a hallmark of RCC."
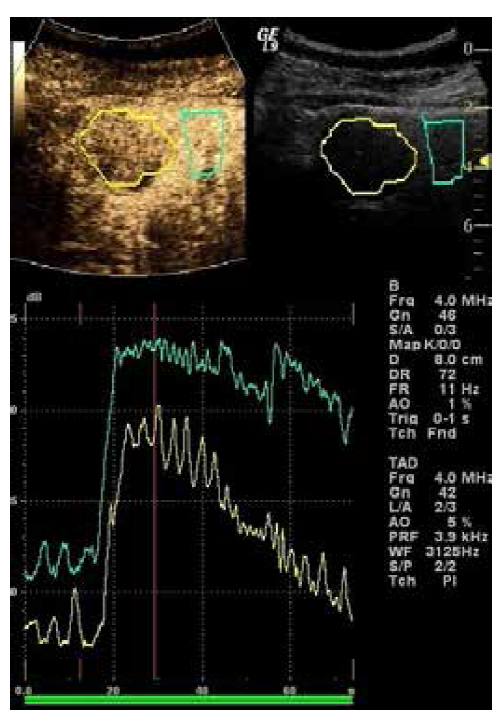
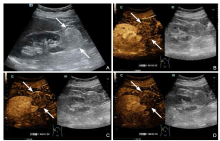
Figure 6
In a 54-year-old female, a hyperechoic mass of 4.9 × 4.3 cm was seen in the lower pole of the right kidney, with clear boundary and regular shape, and part of it protrudes out of the renal capsule (A). After intravenous injection of ultrasound contrast agent SonoVue, homogenous iso- and hypo-enhancement seen in the cortical (B) and the medullary (C) phases, and very low enhancement seen at the delayed phase (D)."
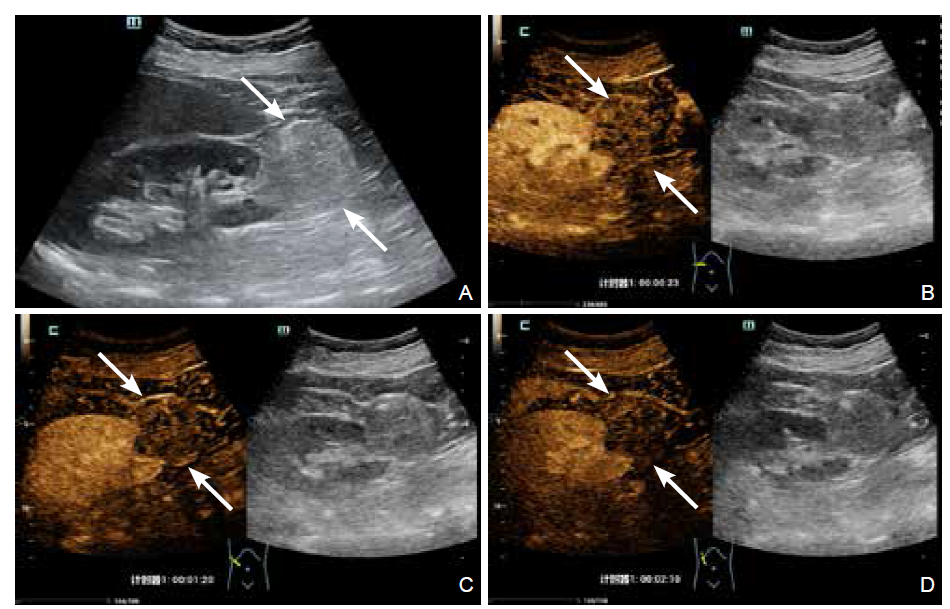
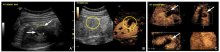
Figure 7
Example of 2D and 3D CEUS of a Multilocular renal cyst. (A) Grey-scale ultrasound shows an anechoic multicystic mass with thin echogenic wall and septa (white arrows); (B) 2D dual imaging shows enhancement of wall and septation during the arterial phase (25 sec post-UCA injection); (C) Continuous CEUS 3D imaging was subsequently performed following a second bolus injection. The multilocular cyst is well visualized in three orthogonal planes (white arrows) and in the volumetric reconstruction (bottom right panel)."
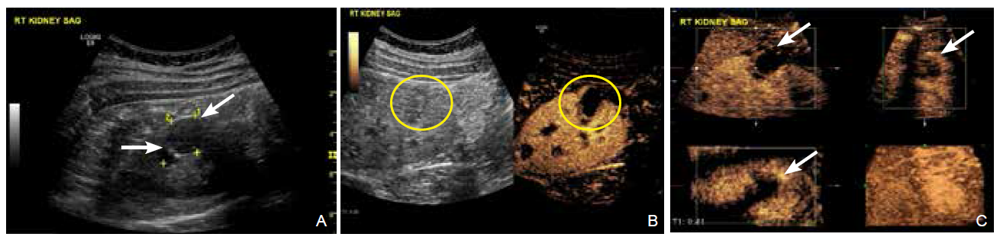

Figure 8
Example of 2D and 3D CEUS of a Clear cell RCC with cystic features. (A) Grey-scale image demonstrating a hypoechogenic 3 × 2.9 cm renal mass; (B) 2D dual imaging shows a diffuse, heterogeneous enhanced tumor with both solid and cystic components during the arterial phase (37 seconds post-UCA injection); (C) Continuous CEUS 3D imaging was subsequently performed following a second bolus injection. The tumor is well visualized in three orthogonal planes (white arrows) and in the volumetric reconstruction (bottom right panel)."
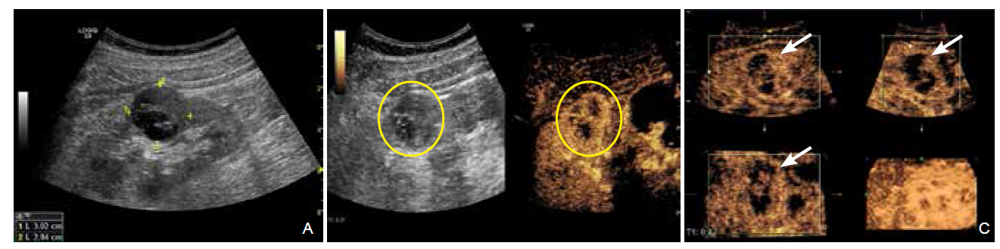
Table 1
Bosniak classification system"
| Class | Description | Features on CE-CT | Malignant risk | Recommendation |
|---|---|---|---|---|
| I | Simple cyst | Anechoic, imperceptible wall, round or oval | < 1% | No follow-up required |
| II | Minimally complex | Single thin septations (<1mm), fine calcification, small diameter (<3cm) | < 3% | No follow-up required |
| IIF | Minimally complex (follow-up recommended) | Multiple thin septations, thick calcification, no contrast enhancement | 5 - 10% | USG or CT follow-up |
| III | Indeterminate | Thick septation, mural nodules, contrast enhancement | 40 - 60% | Surgical excision |
| IV | Clearly malignant | Solid enhancing elements, large cystic components, irregular margins, prominent nodules | 80 - 100% | Surgical excision |
Table 2
Modified bosniak classification system using CEUS"
| Class | Description | Proposed work-up |
|---|---|---|
| I | Simple cyst | No further work-up. |
| II or IIF | Minimally complex | Evaluate cyst enhancement with UCA: |
| ● No enhancement: no further follow-up needed. | ||
| ● Substantial enhancement: assess with CT. Even if CT is negative for enhancement, consider ultrasound follow-up. | ||
| III | Indeterminate | Evaluate cyst enhancement with UCA: |
| IV | Clearly malignant | ● No enhancement: assess with CT. Then follow-up with US. |
| ● Substantial enhancement: consider surgery. Follow-up is mandatory if surgery is not performed. |

Figure 9
Example of 2D and 3D CEUS of a 2.5 cm ablation cavity (white arrows) 18 months post cryoablation. (A) 2D dual imaging shows no enhancement within the ablation cavity during the arterial phase (39 seconds post injection of 1ml Optison, GE Healthcare); (B) Similar lack of enhancement on 2D CEUS is observed in the later phases (1:07 post injection); (C) Continuous 3D imaging was subsequently performed following a second 1 ml bolus injection. The ablation cavity is well visualized in three orthogonal planes (white arrows) and in the volumetric reconstruction (bottom right panel); (D) Post-processing was then performed to evaluate the volume on a slice by slice basis with slice distances of 1.3 mm in order to confirm lack of enhancement throughout the cavity."
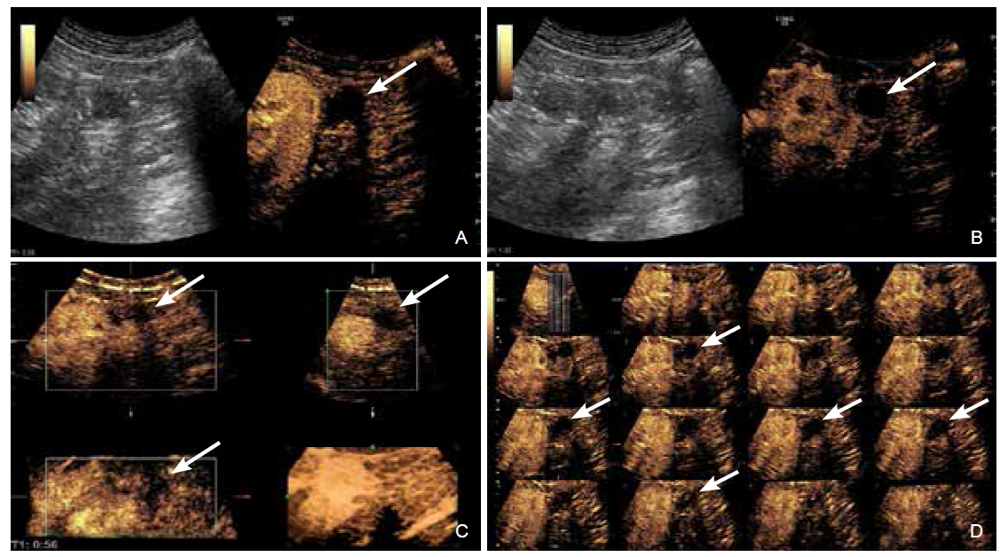

Figure 10
A 29-year-old man with 19-year diabetes and renal failure underwent combined pancreas-kidney transplantation. (A) At 19 days after transplantation with a creatinine of 556umol/L, Doppler ultrasound showed a high-resistance reverse flow of renal artery during diastole; (B-D) Contrast-enhanced ultrasound displayed apparent filling of the renal artery and its branches with no evident signs of venous return, consistent with renal vein occlusion."
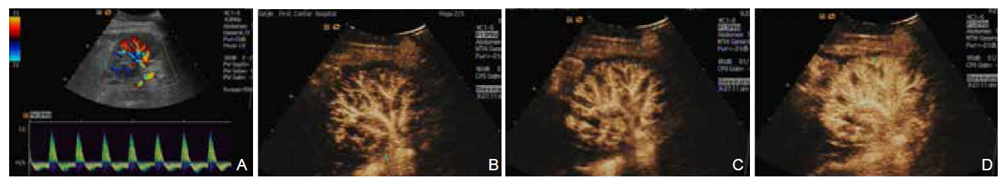
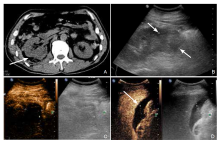
Figure 11
Kidney injury in a 23-year-old female patient involved in a traffic accident. (A) CT scan showed a low-density mass without a clear boundary in the lower pole of the right kidney (arrow); (B) Gray-scale ultrasound image at the same region in figure A showed a complex mass (white arrows); (C) CEUS imaging showed the lesion without enhancement (perfusion defect denoted by marks, 2.5 × 1.8 × 2.5 cm). No active bleeding was identified during the CEUS exam; (D) An unenhanced fluid collection (white arrows) was seen under the left lobe of the liver."
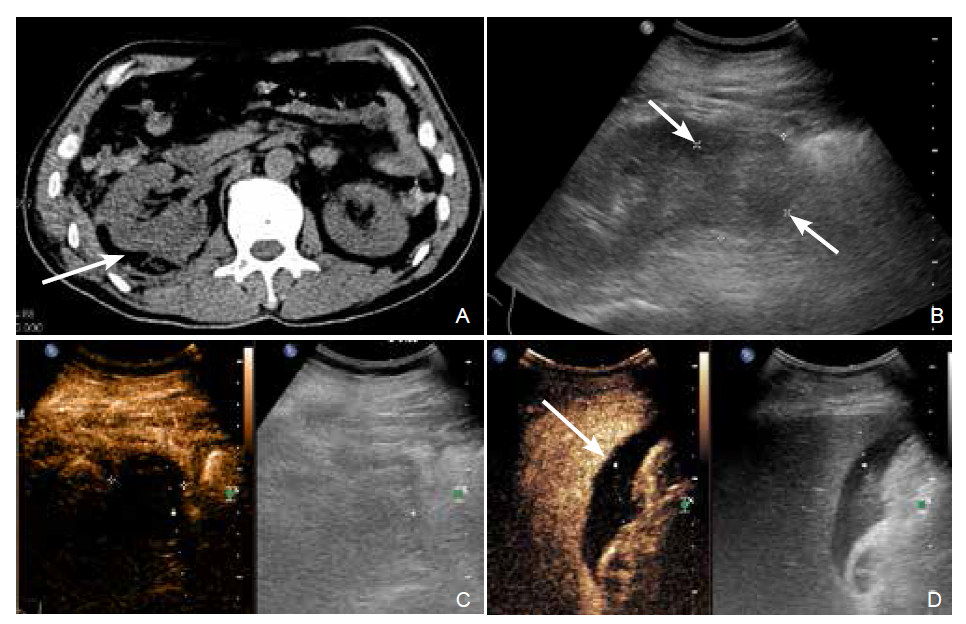
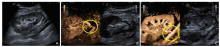
Figure 12
A 33-year-old male patient who had elevated creatinine for 4 years was diagnosed with chronic renal failure-uremic stage and underwent kidney transplantation. Ultrasound was performed 10 days after kidney transplantation with a creatinine of 130umol/L. (A) Gray-scale ultrasound showed that the size and shape of the transplanted kidney were average, and the demarcation between the cortex and medulla was clear; (B-C) Contrast-enhanced ultrasound showed a narrowed segment of the renal artery branch at the lower pole, with a diameter of about 0.3 cm, suggesting the presence of renal artery stenosis in the transplanted kidney."


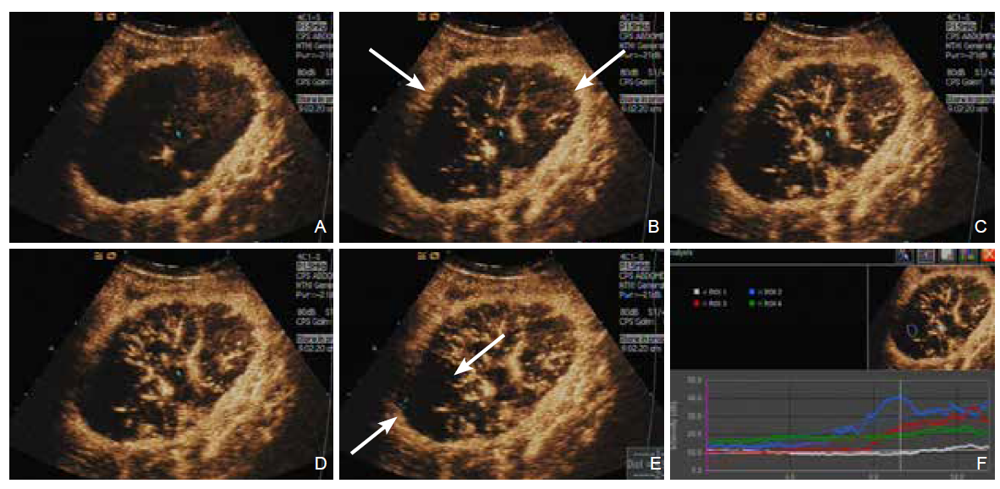
Figure 13
A 62-year-old man underwent kidney transplantation for chronic renal failure. Presented with oliguria for over 2 months and creatinine of 638umol/L. Real-time CEUS was used to see renal perfusion status. (A) Before contrast injection; (B) 12 sec after contrast injection, the capsule of the transplanted kidney was enhanced (white arrows); (C-D) 14 sec after injection, the main renal artery and the intrarenal segment arteries were enhanced gradually and visualized sequentially; (E-F) The upper pole of renal parenchyma identified a non-perfusion area (white arrows) measuring 4.9 × 4.3 × 4.0 cm and irregular enhancement within the kidney, consisting of a localized renal infarction and inhomogeneous hypoperfusion status."
| [1] |
Aggarwal A, Goswami S, Das CJ. Contrast-enhanced ultrasound of the kidneys: principles and potential application. Abdom Radiol (NY) 2022; 47:1369-1384.
doi: 10.1007/s00261-022-03438-z pmid: 35150315 |
| [2] | Granata A, Campo I, Lentini P, Pesce F, Gesualdo L, Basile A, et al. Role of contrast-enhanced ultrasound (CEUS) in native kidney pathology: limits and fields of actio. Diagnostics (Basel) 2021; 11:1058. |
| [3] |
Fröhlich E, Muller R, Cui XW, Schreiber-Dietrich D, Dietrich CF. Dynamic contrast-enhanced ultrasound for quantification of tissue perfusio. J Ultrasound Med 2015; 34:179-196.
doi: 10.7863/ultra.34.2.179 pmid: 25614391 |
| [4] |
Dietrich CF, Averkiou M, Nielsen MB, Barr RG, Burns PN, Calliada F, et al How to perform contrast-enhanced ultrasound (CEUS). Ultrasound Int Open 2018; 4:E2-E15.
doi: 10.1055/s-0043-123931 |
| [5] |
Eisenbrey JR, Forsberg F, Wessner CE, Delaney LJ, Bradigan K, Gummadi S, et al. US-triggered microbubble destruction for augmenting hepatocellular carcinoma response to transarterial radioembolization: a randomized pilot clinical tria. Radiology 2021; 298:450-457.
doi: 10.1148/radiol.2020202321 pmid: 33320067 |
| [6] |
Weber MA, Krix M, Delorme S. Quantitative evaluation of muscle perfusion with CEUS and with M. Eur Radiol 2007; 17:2663-2674.
doi: 10.1007/s00330-007-0641-y |
| [7] |
Greis C. Quantitative evaluation of microvascular blood flow by contrast-enhanced ultrasound (CEUS..Clin Hemorheol Microcirc 2011; 49:137-149.
doi: 10.3233/CH-2011-1464 |
| [8] |
Eisenbrey JR, Kamaya A, Gummadi S, Bird K, Burrowes D, Arias D, et al. Effects of contrast-enhanced ultrasound of indeterminate renal masses on patient clinical management: retrospective analysis from 2 institution. J Ultrasound Med 2021; 40:131-139.
doi: 10.1002/jum.15383 |
| [9] |
Chang EH. An introduction to contrast-enhanced ultrasound for nephrologist. Nephron 2018; 138:176-185.
doi: 10.1159/000484635 |
| [10] |
Main ML, Goldman JH, Grayburn PA. Ultrasound contrast agents: balancing safety versus efficac. Expert Opin Drug Saf 2009; 8:49-56.
doi: 10.1517/14740330802658581 |
| [11] |
Roberts VH, Frias AE. Contrast-enhanced ultrasound for the assessment of placental development and functio. Biotechniques 2020; 69:392-399.
doi: 10.2144/btn-2020-0069 |
| [12] |
Faccioli N, Dietrich CF, Foti G, Santi E, Comai A, D'Onofrio M. Activity-based cost analysis of including contrast-enhanced ultrasound (CEUS) in the diagnostic pathway of focal pancreatic lesions detected by abdominal ultrasoun. Ultraschall Med 2019; 40:618-624. English.
doi: 10.1055/a-0869-7861 pmid: 30895585 |
| [13] |
Streb JW, Tchelepi H, Malhi H, Deurdulian C, Grant EG. Retrospective analysis of contrast-enhanced ultrasonography effectiveness in reducing time to diagnosis and imaging-related expenditures at a single large united states county hospita. Ultrasound Q 2019; 35:99-102.
doi: 10.1097/RUQ.0000000000000375 |
| [14] |
Robbin ML, Lockhart ME, Barr RG. Renal imaging with ultrasound contrast: current statu. Radiol Clin North Am 2003; 41:963-978.
doi: 10.1016/S0033-8389(03)00070-8 |
| [15] |
Ignee A, Straub B, Schuessler G, Dietrich CF. Contrast enhanced ultrasound of renal masse. World J Radiol 2010; 2:15-31.
doi: 10.4329/wjr.v2.i1.15 |
| [16] | Barr RG, Peterson C, Hindi A. Evaluation of indeterminate renal masses with contrast-enhanced US: a diagnostic performance stud. Radiology 2014; 271:133-142. |
| [17] |
Zarzour JG, Lockhart ME, West J, Turner E, Jackson BE, Thomas JV, et al. Contrast-enhanced ultrasound classification of previously indeterminate renal lesion. J Ultrasound Med 2017; 36:1819-1827.
doi: 10.1002/jum.14208 |
| [18] |
Rübenthaler J, Negrão de Figueiredo G, Mueller-Peltzer K, Clevert DA. Evaluation of renal lesions using contrast-enhanced ultrasound (CEUS); a 10-year retrospective European single-centre analysi. Eur Radiol 2018; 28:4542-4549.
doi: 10.1007/s00330-018-5504-1 pmid: 29744641 |
| [19] |
Rübenthaler J, Paprottka K, Marcon J, Hameister E, Hoffmann K, Joiko N, et al. Comparison of magnetic resonance imaging (MRI) and contrast-enhanced ultrasound (CEUS) in the evaluation of unclear solid renal lesion. Clin Hemorheol Microcirc 2016; 64:757-763.
doi: 10.3233/CH-168034 |
| [20] |
Whelan TF. Guidelines on the management of renal cyst diseas. Can Urol Assoc J 2010; 4:98-99.
doi: 10.5489/cuaj.799 |
| [21] |
Wile GE, Leyendecker JR, Krehbiel KA, Dyer RB, Zagoria RJ. CT and MR imaging after imaging-guided thermal ablation of renal neoplasm. Radiographics 2007; 27:325-339; discussion 339-340.
doi: 10.1148/rg.272065083 |
| [22] |
Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, Hora M, et al. EAU guidelines on renal cell carcinoma: 2014 updat. Eur Urol 2015; 67:913-924.
doi: 10.1016/j.eururo.2015.01.005 pmid: 25616710 |
| [23] |
Iannuccilli JD, Grand DJ, Dupuy DE, Mayo-Smith WW. Percutaneous ablation for small renal masses-imaging follow-u. Semin Intervent Radiol 2014 ; 31:50-63.
doi: 10.1055/s-0033-1363843 |
| [24] |
Davenport MS, Caoili EM, Cohan RH, Ellis JH, Higgins EJ, Willatt J, et al. MRI and CT characteristics of successfully ablated renal masses: Imaging surveillance after radiofrequency ablatio. AJR Am J Roentgenol 2009; 192:1571-1578.
doi: 10.2214/AJR.08.1303 |
| [25] |
Eisenbrey JR, Shaw CM, Lyshchik A, Machado P, Lallas CD, Trabulsi EJ, et al. Contrast-enhanced subharmonic and harmonic ultrasound of renal masses undergoing percutaneous cryoablatio. Acad Radiol 2015; 22:820-826.
doi: 10.1016/j.acra.2015.03.008 pmid: 25882093 |
| [26] |
Meloni MF, Bertolotto M, Alberzoni C, Lazzaroni S, Filice C, Livraghi T, et al. Follow-up after percutaneous radiofrequency ablation of renal cell carcinoma: contrast-enhanced sonography versus contrast-enhanced CT or MRI. AJR Am J Roentgenol 2008; 191:1233-1238.
doi: 10.2214/AJR.07.3238 |
| [27] | Tzou DT, Weinstein S, Usawachintachit M, Mongan J, Greene KL, Chi T. Contrast enhanced ultrasound detects recurrent renal cell carcinoma in the setting of chronic renal insufficienc. Clin Genitourin Cancer 2017; 15:e735-e737. |
| [28] | Guo F, Hu B, Chen L, Li J. Clinical application of contrast-enhanced ultrasound after percutaneous renal tumor ablatio. Br J Radiol 2019; 92:20190183. |
| [29] |
Calio BP, Lyshchik A, Li J, Stanczak M, Shaw CM, Adamo R, et al. Long term surveillance of renal cell carcinoma recurrence following ablation using 2D and 3D contrast-enhanced ultrasoun. Urology 2018; 121:189-196.
doi: 10.1016/j.urology.2018.05.053 |
| [30] |
Sugi MD, Joshi G, Maddu KK, Dahiya N, Menias CO. Imaging of renal transplant complications throughout the life of the allograft: comprehensive multimodality revie. Radiographics 2019; 39:1327-1355.
doi: 10.1148/rg.2019190096 |
| [31] | Franke D, Daugherty RJ, Ključevšek D, Ntoulia A, Rafailidis V, Takahashi MS, et al. Contrast-enhanced ultrasound of transplant organs - liver and kidney - in children. Pediatr Radiol2021;51:2284-2302. |
| [32] |
Hai Y, Chong W, Liu JB, Forsberg F, Eisenbrey J. The diagnostic value of contrast-enhanced ultrasound for monitoring complications after kidney transplantation-a systematic review and meta-analysi. Acad Radiol 2021; 28:1086-1093..
doi: 10.1016/j.acra.2020.05.009 |
| [33] |
Mueller-Peltzer K, Rübenthaler J, Fischereder M, Habicht A, Reiser M, Clevert DA. The diagnostic value of contrast-enhanced ultrasound (CEUS) as a new technique for imaging of vascular complications in renal transplants compared to standard imaging modalitie. Clin Hemorheol Microcirc 2017; 67:407-413.
doi: 10.3233/CH-179221 |
| [34] |
Sharfuddin A. Renal relevant radiology: imaging in kidney transplantatio. Clin J Am Soc Nephrol 2014; 9:416-429.
doi: 10.2215/CJN.02960313 |
| [35] | Korda D, Deák PÁ, Kozma V, Kiss G, Doros A. Role of contrast-enhanced ultrasound in the follow-up of kidney transplant patients. Transplant Proc2016;48:2544-2547. |
| [36] | Mueller-Peltzer K, Negrão de Figueiredo G, Fischereder M, Habicht A, Rübenthaler J, Clevert DA. Vascular rejection in renal transplant: diagnostic value of contrast-enhanced ultrasound (CEUS) compared to biopsy. Clin Hemorheol Microcirc2018;69:77-82. |
| [37] |
Wei K, Le E, Bin JP, Coggins M, Thorpe J, Kaul S. Quantification of renal blood flow with contrast-enhanced ultrasoun. J Am Coll Cardiol 2001; 37:1135-1140.
pmid: 11263620 |
| [38] |
Srivastava A, Sridharan A, Walmer RW, Kasoji SK, Burke LMB, Dayton PA, et al. Association of contrast-enhanced ultrasound-derived kidney cortical microvascular perfusion with kidney functio.. Kidney360. 2022; 3:647-656.
doi: 10.34067/KID.0005452021 |
| [39] |
Schneider AG, Hofmann L, Wuerzner G, Glatz N, Maillard M, Meuwly JY, et al. Renal perfusion evaluation with contrast-enhanced ultrasonograph. Nephrol Dial Transplant 2012; 27:674-681.
doi: 10.1093/ndt/gfr345 |
| [40] |
Kishimoto N, Mori Y, Nishiue T, Nose A, Kijima Y, Tokoro T, et al. Ultrasound evaluation of valsartan therapy for renal cortical perfusio. Hypertens Res 2004; 27:345-349.
pmid: 15198482 |
| [41] |
Garessus J, Brito W, Loncle N, Vanelli A, Hendriks-Balk M, Wuerzner G, et al. Cortical perfusion as assessed with contrast-enhanced ultrasound is lower in patients with chronic kidney disease than in healthy subjects but increases under low salt condition. Nephrol Dial Transplant 2022; 37:705-712.
doi: 10.1093/ndt/gfab001 |
| [42] |
Schneider A, Johnson L, Goodwin M, Schelleman A, Bellomo R. Bench-to-bedside review: contrast enhanced ultrasonography--a promising technique to assess renal perfusion in the ICU. Crit Care 2011; 15:157.
doi: 10.1186/cc10058 |
| [43] |
Cagini L, Gravante S, Malaspina CM, Cesarano E, Giganti M, Rebonato A, et al. Contrast enhanced ultrasound (CEUS) in blunt abdominal traum. Crit Ultrasound J 2013; 5:S9.
doi: 10.1186/2036-7902-5-S1-S9 |
| [44] | Miele V, Piccolo CL, Galluzzo M, Ianniello S, Sessa B, Trinci M. Contrast-enhanced ultrasound (CEUS) in blunt abdominal traum. Br J Radiol 2016; 89:20150823. |
| [45] |
Brenda E. Tester BS, Ji-Bin Liu, John R. Eisenbrey, George Koenig. Emerging applications of contrast-enhanced ultrasound in traum. Advanced Ultrasound in Diagnosis and Therapy 2022, 6: 39-47.
doi: 10.37015/AUDT.2022.220017 |
| [46] |
Piskunowicz M, Kosiak W, Batko T. Intravenous application of second-generation ultrasound contrast agents in children: a review of the literatur. Ultraschall Med 2012; 33:135-140.
doi: 10.1055/s-0031-1281936 pmid: 22161614 |
| [47] |
Catalano O, Aiani L, Barozzi L, Bokor D, De Marchi A, Faletti C, et al. CEUS in abdominal trauma: multi-center stud. Abdom Imaging 2009 ; 34:225-234.
doi: 10.1007/s00261-008-9452-0 pmid: 18682877 |
| [48] |
Pinto F, Valentino M, Romanini L, Basilico R, Miele V. The role of CEUS in the assessment of haemodynamically stable patients with blunt abdominal traum. Radiol Med 2015; 120:3-11.
doi: 10.1007/s11547-014-0455-3 |
| [49] |
Kummer T, Oh L, Phelan MB, Huang RD, Nomura JT, Adhikari S. Emergency and critical care applications for contrast-enhanced ultrasoun. Am J Emerg Med 2018; 36:1287-1294.
doi: 10.1016/j.ajem.2018.04.044 |
| [50] |
Schäberle W, Leyerer L, Schierling W, Pfister K. Ultrasound diagnostics of renal artery stenosis: Stenosis criteria, CEUS and recurrent in-stent stenosi. Gefasschirurgie 2016; 21:4-13.
pmid: 27034579 |
| [51] | Cui Y, Zhang Q, Yan J, Wu J. The value of contrast-enhanced ultrasound versus doppler ultrasound in grading renal artery stenosi. Biomed Res Int 2020; 2020:7145728. |
| [52] |
Ran X, Lin L, Yang M, Niu G, Chen L, Shao Y, et al. Contrast-enhanced ultrasound evaluation of renal blood perfusion changes after percutaneous transluminal renal angioplasty and stenting for severe atherosclerotic renal artery stenosi. Ultrasound Med Biol 2020; 46:1872-1879.
doi: S0301-5629(20)30177-0 pmid: 32451193 |
| [53] | Claudon M, Plouin PF, Baxter GM, Rohban T, Devos DM. Renal arteries in patients at risk of renal arterial stenosis: multicenter evaluation of the echo-enhancer SH U 508A at color and spectral Doppler US. Levovist Renal Artery Stenosis Study Group. Radiology 2000; 214:739-746. |
| [54] |
Bertolotto, Michele and Orlando Catalano. “Contrast-enhanced Ultrasound: Past, Present, and Future”. Ultrasound Clinics 4 (2009): 339-367.
doi: 10.1016/j.cult.2009.10.011 |
| [55] |
Siracusano S, Bertolotto M, Ciciliato S, Valentino M, Liguori G, Visalli F. The current role of contrast-enhanced ultrasound (CEUS) imaging in the evaluation of renal patholog. World J Urol 2011; 29:633-638.
doi: 10.1007/s00345-011-0699-7 pmid: 21604017 |
| [56] |
Bertolotto M, Martegani A, Aiani L, Zappetti R, Cernic S, Cova MA. Value of contrast-enhanced ultrasonography for detecting renal infarcts proven by contrast enhanced CT. A feasibility stud. Eur Radiol 2008; 18:376-383.
pmid: 17851664 |
| [57] |
Kazmierski B, Deurdulian C, Tchelepi H, Grant EG. Applications of contrast-enhanced ultrasound in the kidne. Abdom Radiol (NY) 2018; 43:880-898.
doi: 10.1007/s00261-017-1307-0 pmid: 28856401 |
| [58] | Fontanilla T, Minaya J, Cortés C, Hernando CG, Arangüena RP, Arriaga J, et al. Acute complicated pyelonephritis: contrast-enhanced ultrasound. Abdom Imaging2012;37:639-646. |
| [59] |
Mitterberger M, Pinggera GM, Colleselli D, Bartsch G, Strasser H, Steppan I, et al. Acute pyelonephritis: comparison of diagnosis with computed tomography and contrast-enhanced ultrasonograph. BJU Int 2008; 101:341-344.
pmid: 17941932 |
| [60] | Hains DS, Cohen HL, McCarville MB, Ellison EE, Huffman A, Glass S, et al. Elucidation of renal scars in children with vesicoureteral reflux using contrast-enhanced ultrasound: a pilot stud. Kidney Int Rep 2017; 2:420-424. |
| [61] |
Huang DY, Yusuf GT, Daneshi M, Ramnarine R, Deganello A, Sellars ME, et al. Contrast-enhanced ultrasound (CEUS) in abdominal interventio. Abdom Radiol (NY) 2018; 43:960-976.
doi: 10.1007/s00261-018-1473-8 pmid: 29450615 |
| [62] | Del Cura JL, Del Cura G, Zabala R, Korta I. Contrast-enhanced ultrasonography to guide diagnostic and therapeutic interventional procedure. Radiologia (Engl Ed):S0033-8338(21)00067-9. English, Spanish. |
| [63] | Huang DY, Yusuf GT, Daneshi M, Husainy MA, Ramnarine R, Sellars ME, et al. Contrast-enhanced US-guided Interventions: improving success rate and avoiding complications using US contrast agent. Radiographics 2017; 37:652-664. |
| [64] |
Dayton PA, Rychak JJ. Molecular ultrasound imaging using microbubble contrast agent. Front Biosci 2007; 12:5124-5142.
doi: 10.2741/2553 |
| [65] |
Postema M, Gilja OH. Contrast-enhanced and targeted ultrasoun. World J Gastroenterol 2011; 17:28-41.
doi: 10.3748/wjg.v17.i1.28 |
| [66] |
Deshpande N, Needles A, Willmann JK. Molecular ultrasound imaging: current status and future direction. Clin Radiol 2010; 65:567-581.
doi: 10.1016/j.crad.2010.02.013 pmid: 20541656 |
| [67] |
Lyshchik A, Fleischer AC, Huamani J, Hallahan DE, Brissova M, Gore JC. Molecular imaging of vascular endothelial growth factor receptor 2 expression using targeted contrast-enhanced high-frequency ultrasonograph. J Ultrasound Med 2007; 26:1575-1586.
doi: 10.7863/jum.2007.26.11.1575 pmid: 17957052 |
| [68] |
Lee DJ, Lyshchik A, Huamani J, Hallahan DE, Fleischer AC. Relationship between retention of a vascular endothelial growth factor receptor 2 (VEGFR2)-targeted ultrasonographic contrast agent and the level of VEGFR2 expression in an in vivo breast cancer mode. J Ultrasound Med 2008; 27:855-866.
doi: 10.7863/jum.2008.27.6.855 |
| [69] | Willmann JK, Lutz AM, Paulmurugan R, Patel MR, Chu P, Rosenberg J, et al. Dual-targeted contrast agent for US assessment of tumor angiogenesis in viv. Radiology 2008; 248:936-944. |
| [70] |
Willmann JK, Bonomo L, Testa AC, Rinaldi P, Rindi G, Valluru KS, et al. Ultrasound molecular imaging with BR55 in patients with breast and ovarian lesions: first-in-human result. J Clin Oncol 2017; 35:2133-2140.
doi: 10.1200/JCO.2016.70.8594 pmid: 28291391 |
| [71] |
Hudson JM, Williams R, Tremblay-Darveau C, Sheeran PS, Milot L, Bjarnason GA, et al. Dynamic contrast enhanced ultrasound for therapy monitorin. Eur J Radiol 2015; 84:1650-1657.
doi: 10.1016/j.ejrad.2015.05.013 pmid: 26231046 |
| [72] | Lassau N, Chami L, Benatsou B, Peronneau P, Roche A. Dynamic contrast-enhanced ultrasonography (DCE-US) with quantification of tumor perfusion: a new diagnostic tool to evaluate the early effects of antiangiogenic treatmen. Eur Radiol 2007; 17:F89-98. |
| [73] |
Sridharan A, Eisenbrey JR, Stanczak M, Machado P, Merton DA, Wilkes A, et al. Characterizing breast lesions using quantitative parametric 3D subharmonic imaging: a multicenter stud. Acad Radiol 2020; 27:1065-1074.
doi: S1076-6332(19)30547-1 pmid: 31859210 |
| [74] | M Carr, C Shaw, K Nam, M Stanczak, A Lyshchik, F Forsberg, Abstract No. 31 - monitoring postablation renal cellular carcinoma using 3D contrast enhanced ultrasound and time intensity curve analysis: preliminary results. Journal of Vascular and Interventional Radiology 2017;28; S16. |
| [75] |
Jung EM, Clevert DA, Schreyer AG, Schmitt S, Rennert J, Kubale R, et al. Evaluation of quantitative contrast harmonic imaging to assess malignancy of liver tumors: a prospective controlled two-center stud. World J Gastroenterol 2007; 13:6356-6364.
doi: 10.3748/wjg.v13.i47.6356 |
| [76] |
Dietrich C, Hartung E, Ignee A. The use of contrast-enhanced ultrasound in patients with GIST metastases that are negative in CT and PET. Ultraschall Med 2008; 29:276-277.
doi: 10.1055/s-2008-1027878 |
| [77] |
McCarville MB, Coleman JL, Guo J, Li Y, Li X, Honnoll PJ, et al. Use of quantitative dynamic contrast-enhanced ultrasound to assess response to antiangiogenic therapy in children and adolescents with solid malignancies: a pilot stud. AJR Am J Roentgenol 2016; 206:933-939.
doi: 10.2214/AJR.15.15789 |
| [78] |
Ma F, Cang Y, Zhao B, Liu Y, Wang C, Liu B, et al. Contrast-enhanced ultrasound with SonoVue could accurately assess the renal microvascular perfusion in diabetic kidney damag. Nephrol Dial Transplant 2012; 27:2891-2898.
doi: 10.1093/ndt/gfr789 |
| [79] |
Huang C, Zhang W, Gong P, Lok UW, Tang S, Yin T, et al. Super-resolution ultrasound localization microscopy based on a high frame-rate clinical ultrasound scanner: an in-human feasibility stud. Phys Med Biol 2021; 66: 10.1088/1361-6560/abef45.
doi: 10.1088/1361-6560/abef45. |
| [80] |
Opacic T, Dencks S, Theek B, Piepenbrock M, Ackermann D, Rix A, et al. Motion model ultrasound localization microscopy for preclinical and clinical multiparametric tumor characterizatio. Nat Commun 2018; 9:1527.
doi: 10.1038/s41467-018-03973-8 pmid: 29670096 |
| [81] |
Christensen-Jeffries K, Couture O, Dayton PA, Eldar YC, Hynynen K, Kiessling F, et al. Super-resolution ultrasound imagin. Ultrasound Med Biol 2020; 46:865-891.
doi: S0301-5629(19)31595-9 pmid: 31973952 |
| [82] |
Yi HM, Lowerison MR, Song PF, Zhang W. A review of clinical applications for super-resolution ultrasound localization microscop. Curr Med Sci 2022; 42:1-16.
doi: 10.1007/s11596-021-2459-2 |
| [83] |
Errico C, Pierre J, Pezet S, Desailly Y, Lenkei Z, Couture O, et al. Ultrafast ultrasound localization microscopy for deep super-resolution vascular imagin. Nature 2015; 527:499-502.
doi: 10.1038/nature16066 |
| [84] | Zhang G, Harput S, Hu H, Christensen-Jeffries K, Zhu J, Brown J, et al. Fast acoustic wave sparsely activated localization microscopy (fast-AWSALM): ultrasound super-resolution using plane-wave activation of nanodroplet. IEEE Trans Ultrason Ferroelectr Freq Control 2019. |
| [85] | Andersen SB, Taghavi I, Søgaard SB, Hoyos CAV, Nielsen MB, Jensen JA, et al. Super-resolution ultrasound imaging can quantify alterations in microbubble velocities in the renal vasculature of rat. Diagnostics (Basel) 2022; 12:1111. |
| [86] |
Chen Q, Yu J, Rush BM, Stocker SD, Tan RJ, Kim K. Ultrasound super-resolution imaging provides a noninvasive assessment of renal microvasculature changes during mouse acute kidney injur. Kidney Int 2020; 98:355-365.
doi: 10.1016/j.kint.2020.02.011 |
| [87] |
Fischer K, Meral FC, Zhang Y, Vangel MG, Jolesz FA, Ichimura T, et al. High-resolution renal perfusion mapping using contrast-enhanced ultrasonography in ischemia-reperfusion injury monitors changes in renal microperfusio. Kidney Int 2016; 89:1388-1398.
doi: 10.1016/j.kint.2016.02.004 |
| [88] |
Huang C, Lowerison MR, Trzasko JD, Manduca A, Bresler Y, Tang S, et al. Short acquisition time super-resolution ultrasound microvessel imaging via microbubble separatio. Sci Rep 2020; 10:6007.
doi: 10.1038/s41598-020-62898-9 |
| [1] | Priscilla Machado, MD, Ji-Bin Liu, MD, Flemming Forsberg, PhD. Sentinel Lymph Node Identification Using Contrast Lymphosonography: A Systematic Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(1): 1-7. |
| [2] | Ping Wang, MM, Yuqun Luo, MM, Yunkai Li, MM, Wensheng Yue, MD, Duo Huang, MD, Xuemei Lin, MM, Shaoli Xie, MM, Bin Xiong, MM. A Misdiagnosed Cervical Vagal Schwannoma: A Case Report and Review of Its Imaging Features and Differential Diagnosis [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(1): 53-56. |
| [3] | Yanling Chen, MM, Hantao Wang, MM, Hong Han, PhD, Yi Dong, PhD, Wen-ping Wang, MD. Contrast-enhanced Ultrasound of Undifferentiated Embryonal Sarcoma of the Liver in Adult: Two Cases Report and Literature Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(4): 204-209. |
| [4] | Huolin Ye, MD, Qiannan Huang, MD, Qingjing Zeng, MD, Xuqi He, MD, Erjiao Xu, MD, Yinglin Long, MD, Kai Li, MD, Rongqin Zheng, MD. Contrast-enhanced Ultrasound for Evaluation of Active Needle Tract Bleeding during Thermal Ablation of Liver Cancer [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(3): 104-111. |
| [5] | Brenda E. Tester, BS, MS, Ji-Bin Liu, MD, John R. Eisenbrey, PhD, George Koenig, MD. Emerging Applications of Contrast-enhanced Ultrasound in Trauma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(2): 39-47. |
| [6] | Xuehong Diao, MD, Lin Chen, MD, Bo Yu, MS, Jiamei Jin, MS, Jia Zhan, MD, Yue Chen, BS. Follicular Thyroid Neoplasmon Conventional and Contrast-enhanced Ultrasound [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(2): 48-57. |
| [7] | Tong Zhang, MD, Xiaolin Yin, Shuang Zheng, MD, Mingwei Sui, MD, Dezhi Zhang, MD. Application Value of Two-Dimensional Ultrasound Combined with Contrast-Enhanced Ultrasound for the Diagnosis of Multiple Bile Duct Hamartomas: A Case Report [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(4): 317-320. |
| [8] | Esika Savsani, Mohamed Tantawi, MD, Corinne E. Wessner, MBA, RDMS, RVT, Philip Lee, MD, Andrej Lyshchik, MD, PhD, Kevin Anton, MD, PhD, Colette M. Shaw, MD, Ji-Bin Liu, MD, John R. Eisenbrey, PhD. Contrast-enhanced Ultrasound Assessment of Treatment Response in a Patient with Multifocal Hepatocellular Carcinoma Treated with Transarterial Chemo and Radioembolization [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(3): 254-257. |
| [9] | Danni He, MS, Qiao Ji, MD, Huitong Lin, MD, Xuankun Liang, MM, Lujing Li, MM, Fengping Liang, MM, Xianxiang Wang, MM, Kun Yuan, MS, Zuofeng Xu, MD. A New-Designed Microwave Ablation System: Testing in ex vivo and in vivo Liver Model [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(1): 39-46. |
| [10] | Mohamed Tantawi, MD, Ji-Bin Liu, MD, John R Eisenbrey, PhD. Recent Advances in Microbubble-Augmented Cancer Therapy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(3): 155-168. |
| [11] | Qiuyang Li, MD, Ying Zhang, MD, Yong Song, MD, Aitao Guo, MD, Nan Li, BS, Yukun Luo, MD, Jie Tang, MD. Clinical Application of Ultrasound in the Diagnosis and Treatment of Reninoma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(3): 211-216. |
| [12] | Qing Zhang, MD, Shuping Wei, MD, Bin Yang, MD, Xiaoqin Qian, MD. Differences Between Type I and Type II Papillary Renal Cell Carcinoma on Ultrasound [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(4): 187-192. |
| [13] | Li Ma, MD, Wenzhao Liang, MD, Yupeng Zhu, MD, Yingqiao Zhu, MD, Dezhi Zhang, MD. Differences in CEUS and CE-MRI Appearance of HCC: A Case Report [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(4): 197-199. |
| [14] | Vishal Thumar, MD, Ji-Bin Liu, MD, John Eisenbrey, PhD. Applications in Molecular Ultrasound Imaging: Present and Future [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(3): 62-75. |
| [15] | Qingyun Song, MD, Sha Hu, Hong Luo, MD, Taizhu Yang, Qianqian Gao, MD, Fan Yang, MD. Contrast-enhanced Ultrasonography: A New Strategy to Confirm Cervical Pregnancy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(3): 123-127. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
Share: WeChat
Copyright ©2018 Advanced Ultrasound in Diagnosis and Therapy
|
 Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
