Advanced Ultrasound in Diagnosis and Therapy ›› 2025, Vol. 9 ›› Issue (2): 154-162.doi: 10.37015/AUDT.2025.240022
• Review Articles • Previous Articles Next Articles
Jiang Lin, Xie Xiaoyan, Xu Ming*( )
)
Received:2024-10-10
Revised:2024-06-02
Accepted:2024-11-18
Online:2025-06-30
Published:2025-07-06
Contact:
Department of Medical Ultrasonics, Institute of Diagnostic and Interventional Ultrasound, The First Affiliated Hospital of Sun Yat-Sen University, No. 58 Zhongshan Er Road, Guangzhou, Guangdong, China e-mail: Jiang Lin, Xie Xiaoyan, Xu Ming. Infectious Complications after Thermal Ablation of Liver Tumors. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 154-162.
Table 1
Common infection sites and pathogens of infectious complications after thermal ablation of liver tumors"
| First author | Country / Region | Year | Number of centers | Ablation technique | Infection incidence | Infection sites | Pathogens |
|---|---|---|---|---|---|---|---|
| Li [ | China | 2023 | 1 | RFA, MWA, laser | 1.1% (80/7545) per procedure | Liver abscess (n = 16), cholangitis (n = 19), cholecystitis (n = 1), ablation zone infection (n = 25), secondary infection with biliary fistula (n = 2), intraperitoneal infection (n = 5), other (n = 12) | Escherichia coli (n = 16), Klebsiella pneumoniae (n = 10), Enterococcus species (n = 4), Staphylococcus species (n = 4), Candida albicans (n = 4), other (n = 9) |
| Shibata [ | Japan | 2003 | 1 | PEI, PMC, RFA | 1.5% (10/683) per procedure (only focused on cholangitis / liver abscess) | Cholangitis (n = 9), liver abscess (n = 8) | Escherichia coli (n = 2), Enterococcus species (n = 2), Klebsiella pneumoniae (n = 1), Enterobacter cloacae (n = 1) |
| Park [ | South Korea | 2017 | 1 | RFA | 1.1% (21/1843) per procedure | Liver abscess (n = 15), cholecystitis (n = 2), skin wound infection (n = 4) | / |
| Koda [ | Japan | 2012 | 20 | RFA | 1.1% (180/16346) per nodule | Liver abscess (n = 32), bile duct dilatation (n = 110), biloma (n = 37), severe acute pancreatitis (n = 1) | / |
| Choi [ | South Korea | 2005 | 1 | RFA | 1.7% (13/751) per procedure (only focused on liver abscess) | Liver abscess (n = 13) | Gram-negative bacilli (n = 3), Enterococcus species (n = 1), Enterococcus faecium (n = 1), Clostridium perfringens (n = 1), Staphylococcus aureus (n = 1) |
| Xiang [ | a meta-analysis including cases from Germany, Japan, China, Switzerland, the USA, South Korea, Austria, England | 2020 | 30 | RFA, MWA, laser | 0.08% (17/2021) per procedure | Liver abscess (n = 6), puncture site infection (n = 7), biloma (n = 4) | / |
| Chen [ | Taiwan, China | 2021 | 1 | RFA | 0.9% (4/452) per procedure (only focused on bacteremia) | Bacteremia (n = 4) | Escherichia coli (n = 2), Klebsiella pneumoniae (n = 1), Staphylococcus epidermidis (n = 1) |
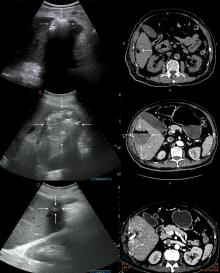
Figure 1
Ultrasound and CT findings of a liver abscess after ablation. An 83-year-old man with hepatocellular carcinoma developed recurrent fever starting on the first day after undergoing RFA. He was subsequently diagnosed with liver abscess based on imaging findings. The patient gradually recovered following treatment with catheter drainage and antibiotics, including cephalosporins and carbapenems. (A) Abdominal ultrasound performed on day 3 after ablation showed hyperechoic gas in the ablation zone of liver S5/6 (arrow); (B) A non-enhanced abdominal CT scan on day 3 after ablation showed the presence of gas in the ablation zone of the liver S5/6 (arrow), without evidence of abscess formation; (C) Abdominal ultrasound on day 20 post-ablation demonstrated an enlarged ablation zone with mixed echogenicity (arrow); (D) An enhanced abdominal CT scan in the arterial phase on day 21 after ablation identified liver abscess (arrow) with thick and rough wall. Part of the abscess wall showed enhancement, and a gas-liquid level was visible within the abscess cavity; (E) Abdominal ultrasound conducted 2 months after ablation showed hyperechoic drainage tubes, with no residual gas in the ablation zone (arrows); (F) An enhanced abdominal CT scan in the arterial phase 2 months after ablation revealed a significantly reduced ablation area in liver S5/6 (arrow). High-density drainage tubes were present within the ablation area."
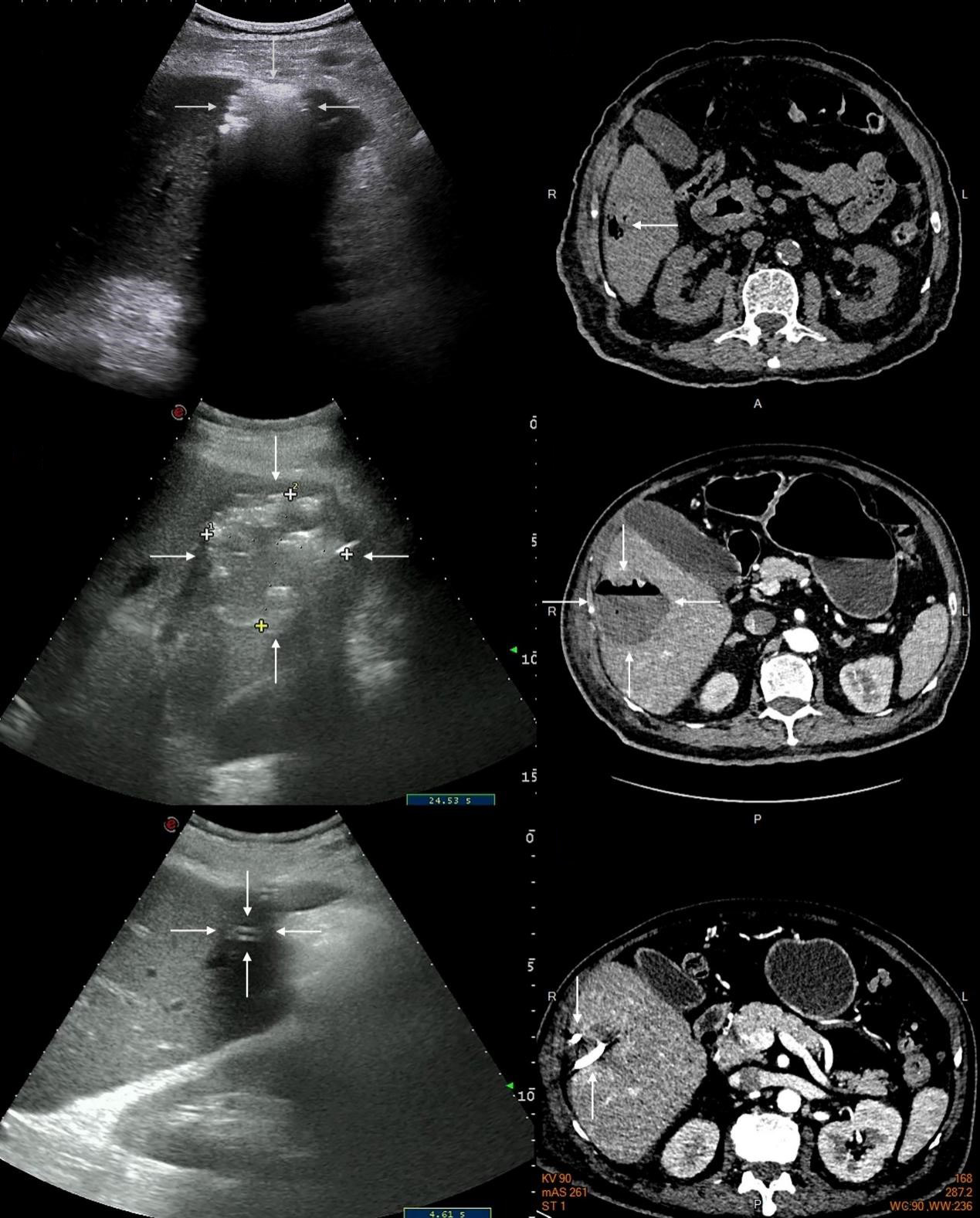
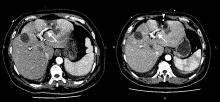
Figure 2
CT findings of post-ablation cholangitis and ablation zone infection. A 55-year-old male with liver metastatic cancer developed high fever and chills on the day after RFA. He was subsequently diagnosed with cholangitis and ablated zone infection based on laboratory tests and CT examination. The patient gradually recovered after receiving catheter drainage and antibiotics therapy, including cephalosporins, carbapenems, and daptomycin. (A) An enhanced abdominal CT scan in the arterial phase on day 5 post-ablation revealed intrahepatic bile duct dilation and gas accumulation, primarily in the left liver (arrow). Gas was also visible in the ablation site in liver S3 (asterisk); (B) An enhanced abdominal CT scan in the arterial phase on day 12 post-ablation showed a reduction in intrahepatic bile duct dilation and gas within bile duct (arrow). However, the gas in the ablation site of liver S3 had increased (asterisk), and a high-density drainage tube was visible at the site (arrowhead)."
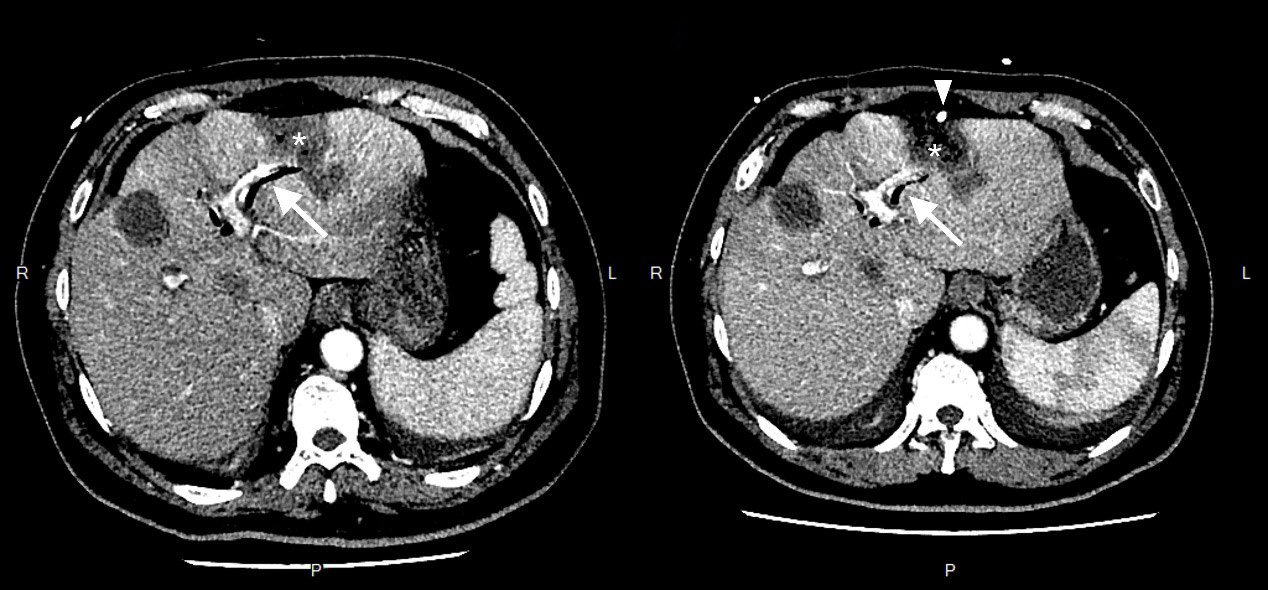
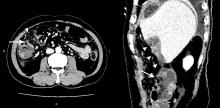
Figure 3
CT findings of peritonitis secondary to colon perforation after ablation. A 68-year-old man with hepatocellular carcinoma developed severe abdominal pain and fever on the day 2 after RFA. Imaging confirmed a diagnosis of intestinal perforation, and the patient underwent emergency surgery. However, the subsequent infection progressed to septic shock. He was transferred to the intensive care unit, where he received catheter drainage, and antifungal (i.e. carpofungine) and antibiotics (i.e. cephalosporins, carbapenems). (A) An axial abdominal enhanced CT scan in the venous phase at day 3 after ablation revealed discontinuity of the intestinal wall at hepatic flexure of colon (arrow), accompanied by surrounding fat standing (arrowhead) and free gas in the peritoneal cavity (asterisk); (B) A sagittal CT recombination image showed perforation site in the colon (arrow), located near subcapsular ablation zone of the liver S6 (arrowhead)."
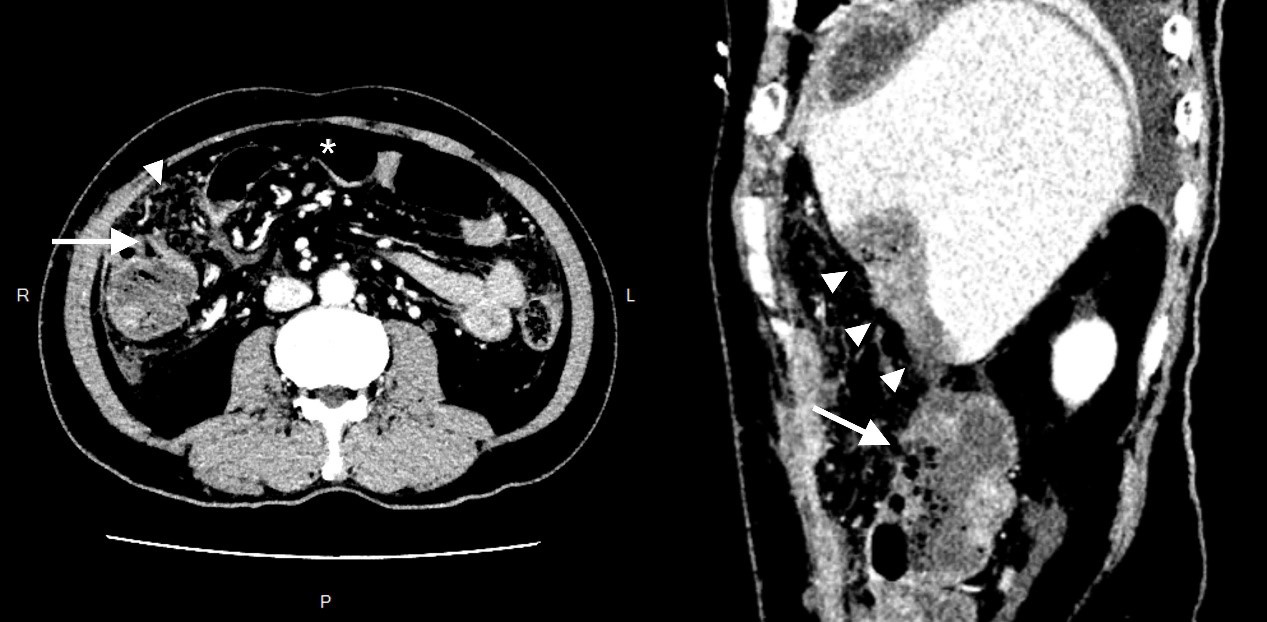
Table 2
Risk factors and predictive models for infection after ablation of liver tumors"
| First author | Country/Region | Year | Outcome for prediction | Risk factors | AUC | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|
| Li [ | China | 2023 | Overall infectious complication | Prior biliary intervention (OR = 18.6), prior TACE (OR = 2.4), the largest tumor size (OR = 1.9) | 0.77 | 0.56 | 0.90 |
| Hepatobiliary infection | Prior biliary intervention (OR = 26.9), prior TACE (OR = 3.6), largest tumor size (OR = 1.7), subcapsular location (OR = 2.6) | 0.82 | 0.64 | 0.88 | |||
| Kwak [ | USA | 2023 | Abscess | A history of Oddi sphincter manipulation (OR = 18.2), cholangiocarcinoma (OR = 13.3), prior TARE †, serum alkaline phosphatase levels † | / | / | / |
| Choi [ | South Korea | 2005 | Liver abscess | Biliary abnormality ‡, treatment with an internally cooled electrode system (OR = 12.4), tumor with retention of iodized oil from previous TACE (OR = 3.4), | / | / | / |
| Shibata [ | Japan | 2003 | Cholangitis and/or liver abscess | Bilioenteric anastomosis (OR = 36.4) | / | / | / |
| Su [ | China | 2016 | Liver abscess | Child-Pugh class B and C (OR = 6.3), porta hepatis tumors (OR = 13.4), biliary tract disease (OR = 6.8), diabetes mellitus (OR = 5.7) | / | / | / |
| Abdelkader [ | Egypt | 2023 | Bacterial infection | Procalcitonin > 0.66 at the 4th day after ablation (OR = ∞) | 1.00 | 1.00 | 1.00 |
| Kang [ | South Korea | 2018 | Bacterial infection in patients with fever | Peak of procalcitonin | 0.84 | / | / |
| Park [ | South Korea | 2017 | Overall infection | Tumor size (OR = 1.4), multiple overlapping ablations (OR = 1.1) | / | / | / |
Table 3
Guidelines or consensus recommendations for prophylactic or therapeutic use of antibiotics for liver tumor ablation"
| Guideline / Consensus | Country/Region | Year | Low-risk patients | High-risk patients | Other |
|---|---|---|---|---|---|
| Practice guidelines for adult antibiotic prophylaxis during vascular and interventional radiology procedures. Written by the Standards of Practice Committee for the Society of Interventional Radiology and Endorsed by the Cardiovascular Interventional Radiological Society of Europe and Canadian Interventional Radiology Association [corrected] [ | USA | 2010 | 1-2 g cefazolin IV | (i) Oral levofloxacin 500 mg/d + oral metronidazole 500 mg BID beginning 2 days before and continuing for 14 days after ablation + oral neomycin 1 g and erythromycin base 1 g at 1, 2, and 11 PM on the day before ablation (ii) 1.5 g ampicillin-sulbactam IV (iii) Vancomycin or clindamycin can be given for gram-positive coverage and gentamicin for gram-negative coverage | / |
| Expert consensus on the application and management of antibiotics in liver tumor ablation (2022 version) [ | China | 2022 | 1.5 g ampicillin-sulbactam IV In patients with penicillin allergy, clindamycin can be given for gram-positive and aminoglycosides can be given for gram-negative | (i) 4.5g piperacillin sodium-tazobactam IV (ii) 2-4 g cefoperazone-sulbactam IV combined with 0.5 g metronidazole IV (iii) 1-2 g ceftriaxone IV combined with 0.5 g metronidazole IV | Carbapenems (such as imipenem, meropenem, etc.) or tigecycline can be used empirically in patients with severe infection. Until the results of the etiological examination are clear, it is necessary to consider the possibility of gram-positive infection, and vancomycin, teicolanin, or linezolid can be given. After the pathogenic bacteria and drug sensitivity were identified, antimicrobial de-escalation should be performed. |
| A guide to antibiotics for the interventional radiologist [ | USA | 2005 | Ceftriaxone or piperacillin-tazobactam or ticarcillin-clavulanic acid or ampicillin-sulbactam, and the dose depends on agent (no risk stratification for patients) | / | |
| [1] | Reig M, Forner A, Rimola J, Ferrer-Fàbrega J, Burrel M, Garcia-Criado Á, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol 2022;76:681-93. |
| [2] | Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol 2016;27:1386-422. |
| [3] | Vogel A, Bridgewater J, Edeline J, Kelley RK, Klümpen HJ, Malka D, et al. Biliary tract cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol 2023;34:127-140. |
| [4] | Awad A, Pal K, Yevich S, Kuban JD, Tam A, Odisio BC, et al. Safety and efficacy of percutaneous image-guided ablation for soft tissue sarcoma metastases to the liver. Cancer 2024;130:2703-2712. |
| [5] | Crocetti L, Lencioni R. Thermal ablation of hepatocellular carcinoma. Cancer imaging 2008;8:19-26. |
| [6] | Xu C, Li L, Xu W, Du C, Yang L, Tong J, et al. Ultrasound-guided percutaneous microwave ablation versus surgical resection for recurrent intrahepatic cholangiocarcinoma: intermediate-term results. Int J Hyperthermia 2019;36:351-358. |
| [7] | van de Geest TW, van Amerongen MJ, Nierop PMH, Höppener DJ, Grünhagen DJ, Moelker A, et al. Propensity score matching demonstrates similar results for radiofrequency ablation compared to surgical resection in colorectal liver metastases. Eur J Surg Oncol 2022;48:1368-1374. |
| [8] | Kang TW, Kim JM, Rhim H, Lee MW, Kim YS, Lim HK, et al. Small hepatocellular carcinoma: radiofrequency ablation versus nonanatomic resection--propensity score analyses of long-term outcomes. Radiology 2015;275:908-919. |
| [9] | Lahat E, Eshkenazy R, Zendel A, Zakai BB, Maor M, Dreznik Y, et al. Complications after percutaneous ablation of liver tumors: a systematic review. Hepatobiliary Surg Nutr 2014;3:317-323. |
| [10] | Qin S, Liu GJ, Huang M, Huang J, Luo Y, Wen Y, et al. The local efficacy and influencing factors of ultrasound-guided percutaneous microwave ablation in colorectal liver metastases: a review of a 4-year experience at a single center. Int J Hyperthermia 2019;36:36-43. |
| [11] | Kulkarni CB, Pullara SK, C SR, Moorthy S. Complications of Percutaneous Radiofrequency Ablation for Hepatocellular Carcinoma. Acad Radiol 2023;31:2987-3003. |
| [12] | Bertot LC, Sato M, Tateishi R, Yoshida H, Koike K. Mortality and complication rates of percutaneous ablative techniques for the treatment of liver tumors: a systematic review. Eur Radiol 2011;21:2584-2596. |
| [13] | Li X, Zhang Y, Wang X, Zeng H, Zhou L, Huang G, et al. Predicting Infectious Complications after Percutaneous Thermal Ablation of Liver Malignancies: A 12-year Single-Center Experience. Radiology 2023;308:e223091. |
| [14] | Shibata T, Yamamoto Y, Yamamoto N, Maetani Y, Shibata T, Ikai I, et al. Cholangitis and liver abscess after percutaneous ablation therapy for liver tumors: incidence and risk factors. J Vasc Interv Radiol. 2003;14:1535-1542. |
| [15] | Park JG, Park SY, Tak WY, Kweon YO, Jang SY, Lee YR, et al. Early complications after percutaneous radiofrequency ablation for hepatocellular carcinoma: an analysis of 1,843 ablations in 1,211 patients in a single centre: experience over 10 years. Clin Radiol 2017;72:692.e9-692.e15. |
| [16] | Koda M, Murawaki Y, Hirooka Y, Kitamoto M, Ono M, Sakaeda H, et al. Complications of radiofrequency ablation for hepatocellular carcinoma in a multicenter study: an analysis of 16 346 treated nodules in 13 283 patients. Hepatol Res 2012;42:1058-1064. |
| [17] | Choi D, Lim HK, Kim MJ, Kim SJ, Kim SH, Lee WJ, et al. Liver abscess after percutaneous radiofrequency ablation for hepatocellular carcinomas: frequency and risk factors. AJR Am J Roentgenol 2005;184:1860-1867. |
| [18] | Kang SJ, Kim UJ, Kim SE, An JH, Jang MO, Myung DS, et al. Predictive value of 0rocalcitonin for bacterial infection after transarterial chemoembolization or radiofrequency ablation for hepatocellular carcinoma. Dis Markers 2018;2018:9120878. |
| [19] | de C Ferreira LE, Baron TH. Acute biliary conditions. Best Pract Res Clin Gastroenterol 2013;27:745-756. |
| [20] | Kiriyama S, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Pitt HA, et al. New diagnostic criteria and severity assessment of acute cholangitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci 2012;19:548-556. |
| [21] | Bréhier G, Besnier L, Delagnes A, Oberti F, Lebigot J, Aubé C, et al. Imaging after percutaneous thermal and non-thermal ablation of hepatic tumour: normal appearances, progression and complications. Br J Radiol 2021;94:20201327. |
| [22] | Kwon HJ, Kim PN, Byun JH, Kim KW, Won HJ, Shin YM, et al. Various complications of percutaneous radiofrequency ablation for hepatic tumors: radiologic findings and technical tips. Acta Radiol 2014;55:1082-1092. |
| [23] | Shakespear JS, Shaaban AM, Rezvani M. CT findings of acute cholecystitis and its complications. AJR Am J Roentgenol 2010;194:1523-1529. |
| [24] | Gerstenmaier JF, Hoang KN, Gibson RN. Contrast-enhanced ultrasound in gallbladder disease: a pictorial review. Abdom Radiol (NY) 2016;41:1640-1652. |
| [25] | Ding R, Zhou J, Yang Y, Zhao L, Luo S, Huang M.A rare complication after radiofrequency ablation in the treatment of colorectal liver metastasis: a case report. J Interv Med 2020;3:213-215. |
| [26] | Roller J, Zimmer V, Bücker A, Glanemann M, Eisele RM.Conservative treatment of gastric perforation after microwave ablation of a hepatocellular carcinoma: case report. Medicine (Baltimore) 2022;101:e29195. |
| [27] | Zhang Y, Li X, Zhang X, Huang T. Analysis of infectious complications after thermal ablation of hepatocellular carcinoma and the impact on long-term survival. Cancers 2022;14:5198. |
| [28] | Livraghi T, Solbiati L, Meloni MF, Gazelle GS, Halpern EF, Goldberg SN. Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology 2003;226:441-451. |
| [29] | Kwak DH, Yu Q, Malavia M, Sellers E, Said A, Patel M, et al. Risk factors for abscess development following percutaneous microwave ablation therapy of hepatic tumors. Cardiovasc Intervent Radiol 2023;46:726-736. |
| [30] | Su XF, Li N, Chen XF, Zhang L, Yan M.Incidence and risk factors for liver abscess after thermal ablation of liver neoplasm. Hepat Mon 2016;16:e34588. |
| [31] | Kobayashi S, Kozaka K, Gabata T, Matsui O, Koda W, Okuda M, et al. Pathophysiology and imaging findings of bile duct necrosis: a rare but serious complication of transarterial therapy for liver tumors. Cancers (Basel) 2020;12:2596. |
| [32] | Chan FS, Ng KK, Poon RT, Yuen J, Tso WK, Fan ST. Duodenopleural fistula formation after percutaneous radiofrequency ablation for recurrent hepatocellular carcinoma. Asian J Surg 2007;30:278-282. |
| [33] | Chang YC, Lin YM.Bronchobiliary fistula after radiofrequency ablation for hepatocellular carcinoma successfully treated by double drainage. Respirol Case Rep 2018;6:e00376. |
| [34] | Pessaux P, van den Broek MA, Wu T, Olde Damink SW, Piardi T, Dejong CH, et al. Identification and validation of risk factors for postoperative infectious complications following hepatectomy. J Gastrointest Surg 2013;17:1907-1916. |
| [35] | Zhang J, Xue F, Liu SD, Liu D, Wu YH, Zhao D, et al. Risk factors and prediction model for inpatient surgical site infection after elective abdominal surgery. World J Gastrointest Surg 2023;15:387-397. |
| [36] | Larkin JG, Frier BM, Ireland JT. Diabetes mellitus and infection. Postgrad Med J 1985;61:233-237. |
| [37] | Abdelkader A, Abdelkhalek R, Hosny H, Emara MH, Elshamy M. Bacterial infections and fever after hepatocellular carcinoma ablation therapy: predictive role of procalcitonin. Clin Exp Hepatol 2023;9:122-128. |
| [38] | Bhatia SS, Spector S, Echenique A, Froud T, Suthar R, Lawson I, et al. Is antibiotic prophylaxis for percutaneous radiofrequency ablation (RFA) of primary liver tumors necessary? results from a single-center experience. Cardiovasc Intervent Radiol 2015;38:922-928. |
| [39] | Tan SL, Yu XL, Liang P, Liu F, Cheng Z, Han ZY, et al. Preventing intrahepatic infection after ablation of liver tumours in biliary-enteric anastomosis patients. Int J Hyperthermia 2017;33:664-669. |
| [40] | Odisio BC, Richter M, Aloia TA, Conrad C, Ahrar K, Gupta S, et al. Use of prophylactic antibiotics to prevent abscess formation following hepatic ablation in patients with prior enterobiliary manipulation. J Gastrointest Surg 2016;20:1428-1434. |
| [41] | The Ablation Expert Committee of the Chinese Society of Clinical Oncology.Expert consensus on the application and management of antibiotics in liver tumor ablation (2022 version). Chinese Journal of Internal Medicine 2022;61:1224-1227. |
| [42] | Lee EJ, Rhim H, Lim HK, Choi D, Lee WJ, Min KS. Effect of artificial ascites on thermal injury to the diaphragm and stomach in radiofrequency ablation of the liver: experimental study with a porcine model. AJR Am J Roentgenol 2008;190:1659-1664. |
| [43] | Kondo Y, Yoshida H, Shiina S, Tateishi R, Teratani T, Omata M. Artificial ascites technique for percutaneous radiofrequency ablation of liver cancer adjacent to the gastrointestinal tract. Br J Surg 2006;93:1277-1282. |
| [44] | Song Y, Wu M, Zhou R, Zhao P, Mao D.Application and evaluation of hydrodissection in microwave ablation of liver tumours in difficult locations. Front Oncol 2023;13:1298757. |
| [45] | Thamtorawat S, Patanawanitkul R, Rojwatcharapibarn S, Chaiyasoot W, Tongdee T, Yodying J, et al. Biliary complications and efficacy after ablation of peribiliary tumors using irreversible electroporation (IRE) or radiofrequency ablation (RFA). Int J Hyperthermia 2022;39:751-757. |
| [46] | Liu J, Li L, Zeng Q, Zheng R, Li K. Prevention of major biliary complications by fusion imaging for thermal ablation of malignant liver tumors adjacent to the bile ducts: a preliminary comparative study. Abdom Radiol (NY) 2022;47:4245-4253. |
| [47] | Wagstaff PG, Buijs M, van den Bos W, de Bruin DM, Zondervan PJ, de la Rosette JJ, et al. Irreversible electroporation: state of the art. Onco Targets Ther 2016;9:2437-2446. |
| [48] | Yu MA, Liang P, Yu XL, Cheng ZG, Han ZY, Liu FY, et al. Liver abscess as a complication of microwave ablation for liver metastatic cholangiocarcinoma after bilioenteric anastomosis. Int J Hyperthermia 2011;27:503-509. |
| [49] | Lai KC, Cheng KS, Jeng LB, Huang CC, Lee YT, Chang HR, et al. Factors associated with treatment failure of percutaneous catheter drainage for pyogenic liver abscess in patients with hepatobiliary-pancreatic cancer. Am J Surg 2013;205:52-57. |
| [50] | Mezhir JJ, Fong Y, Jacks LM, Getrajdman GI, Brody LA, Covey AM, et al. Current management of pyogenic liver abscess: surgery is now second-line treatment. J Am Coll Surg 2010;210:975-983. |
| [51] | Korutz AW, Sato KT. Radiofrequency ablation of a solitary liver metastasis complicated by colonic perforation. Semin Intervent Radiol 2011;28:171-174. |
| [52] | Yasumoto T, Shimizu J, Watanabe N, Inada M, Nakata S, Sato M, et al. [A case of bile peritonitis caused by jejunal perforation after radiofrequency ablation for the multiple liver metastases from cholangiocarcinoma successfully treated with various interventional radiological procedures after pancreatoduodenectomy]. Gan To Kagaku Ryoho 2009;36:2093-2095. |
| [53] | Xiang J, Liu M, Lu R, Wang L, Xu Y, He X, et al. Magnetic resonance-guided ablation of liver tumors: a systematic review and pooled analysis. J Cancer Res Ther 2020;16:1093-1099. |
| [54] | Chen PY, Tsai TJ, Yang HY, Chou CK.The incidence of bacteremia and risk factors of post-radiofrequency ablation fever for patients with hepato-cellular carcinoma. Cancers (Basel) 2021;13:5303. |
| [55] | Venkatesan AM, Kundu S, Sacks D, Wallace MJ, Wojak JC, Rose SC, et al. Practice guidelines for adult antibiotic prophylaxis during vascular and interventional radiology procedures. Written by the Standards of Practice Committee for the Society of Interventional Radiology and endorsed by the Cardiovascular Interventional Radiological Society of Europe and Canadian Interventional Radiology Association [corrected]. J Vasc Interv Radiol 2010;21:1611-1630. |
| [56] | Zarrinpar A, Kerlan RK. A guide to antibiotics for the interventional radiologist. Semin Intervent Radiol 2005;22:69-79. |
| [1] | Liu Tong, Meng Kexin, Zhu Ying, Fan Fengjing, Wang Bei. Clinical Treatment Status of Papillary Thyroid Microcarcinoma [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(1): 41-46. |
| [2] | Lanxia Zhang, MM, Qingjing Zeng, MD, Guanghui Guo, MM, Xuqi He, MM, Kai Li, MD. An Epstein-Barr Virus Positive Lymphoepithelioma-Like Cholangiocarcinoma in A Young Woman with Chronic Hepatitis B Treated through Microwave Ablation: A Case Report and Literature Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2023, 7(4): 405-408. |
| [3] | Huolin Ye, MD, Qiannan Huang, MD, Qingjing Zeng, MD, Xuqi He, MD, Erjiao Xu, MD, Yinglin Long, MD, Kai Li, MD, Rongqin Zheng, MD. Contrast-enhanced Ultrasound for Evaluation of Active Needle Tract Bleeding during Thermal Ablation of Liver Cancer [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(3): 104-111. |
| [4] | Xiaohui Ji, MD, Juanjuan Li, MD, Dongxia Gao, MD. Ultrasound-guided Microwave Ablation of Adenolymphoma of Parotid Gland: A Case Report [J]. Advanced Ultrasound in Diagnosis and Therapy, 2022, 6(1): 22-25. |
| [5] | Yan Zhou, Jianmin Ding, Fengmei Wang, Zhengyi Qin, Yandong Wang, Hongyu Zhou, Xiang Jing. The Effects of Liver Function Damage after Thermal Ablation on the Prognosis of HCC Patients and Its Prediction [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(2): 80-86. |
| [6] | Tong Zhang, MD, Wenzhao Liang, MD, Yuanyuan Song, MD, Zhengmin Wang, MD, Dezhi Zhang, MD. Microwave Ablation of Colorectal Liver Metastases Guided by US-PET/CT Fusion Imaging: A Case Report [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(1): 58-62. |
| [7] | Danni He, MS, Qiao Ji, MD, Huitong Lin, MD, Xuankun Liang, MM, Lujing Li, MM, Fengping Liang, MM, Xianxiang Wang, MM, Kun Yuan, MS, Zuofeng Xu, MD. A New-Designed Microwave Ablation System: Testing in ex vivo and in vivo Liver Model [J]. Advanced Ultrasound in Diagnosis and Therapy, 2021, 5(1): 39-46. |
| [8] | Tong Zhang, MD, Wenzhao Liang, MD, Yuanyuan Song, MD, Zhengmin Wang, MD, Dezhi Zhang, MD. US-CT Fusion Image-Guided Microwave Ablation of Lung Cancer----A New Mode of Image Guidance in Lung Cancer Ablation [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(4): 343-348. |
| [9] | Ruiqing Liu, MD, Yaqiong Li, PhD, Bing Mao, MD, Na Li, PhD, Shaobo Duan, MD, Zhiyang Chang, MS, Ye Zhang, MS, Shuaiyang Wang, MS, Lianzhong Zhang, MD. Focal Ablation Therapy for Prostate Cancer: A Literature Review [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(4): 308-314. |
| [10] | Yuejin Wu, MS, Shaobo Duan, MD, Luwen Liu, MS, Shuaiyang Wang, MS, Shuang Xu, MS, Liuwei Hao, BS, Lianzhong Zhang, MD. Inter-ventricular Septum Ablation for the Treatment of Hypertrophic Obstructive Cardiomyopathy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(4): 297-302. |
| [11] | Jie Chen, MD, Bo Zhang, MD, Mo Yang, MB, Yan Tian, MD, Dandan Guo, MS, Boya Wang, MD, Weidan Lu, MS, Jiaojiao Ma, MS, Cui Zhao, MB, Shuliang Zang, MB, Jianya Wang, MB. Management Strategies of Ultrasound Department in Response to the Epidemic Crisis [J]. Advanced Ultrasound in Diagnosis and Therapy, 2020, 4(2): 90-98. |
| [12] | Shengnan Huo, MD, Lin Yin, Lili Peng, MD, Zhao Wang, MD, Ming-an Yu, MD. Microwave Ablation of An Autonomous Functioning Thyroid Nodule in A Pregnant Patient: A Case Report [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(3): 136-139. |
| [13] | Huijuan Peng, MD, Wenzhao Liang, MD, Lei Liu, MD, Jing Jia, MD, Yingqiao Zhu, Dezhi Zhang, MD. Fusion Image of Gd-EOB-DTPA MRI and Ultrasound Guiding Microwave Ablation of Hepatocellular Carcinoma Adjacent to Intrahepatic Bile Ducts: A Report of Two Cases [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(3): 132-135. |
| [14] | Lei Yan, MM, Jianquan Zhang, MD, Jianguo Sheng, MM, Hang Zhang, MM, Zongping Diao, MM, Jianming Zheng, PhD. The Significance of Heat Shock Protein 70 Expression in Benign Thyroid Nodules During Thermal Ablation [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(3): 103-108. |
| [15] | Bowen Zheng, MD, Tao Wu, MD, Ying Ruan, MD, Jun Chen, MD, Jie Ren, MD. Inflammation Spreading from Subacute Thyroiditis Following Fine-needle Aspiration: A Case Report [J]. Advanced Ultrasound in Diagnosis and Therapy, 2019, 3(2): 50-52. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
Share: WeChat
Copyright ©2018 Advanced Ultrasound in Diagnosis and Therapy
|
 Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
