Consensus and Guidelines
- Chinese Expert Consensus on Critical Care Ultrasound Applications at COVID-19 Pandemic
- Faqin Lv, MD, Jinrui Wang, MD, Xing Yu, MD, Aiping Yang, MD, Ji-Bin Liu, MD, Linxue Qian, MD, Huixiong Xu, MD, Ligang Cui, MD, Mingxing Xie, MD, Xi Liu, MD, Chengzhong Peng, MD, Yi Huang, MD, Haiyan Kou, MD, Shengzheng Wu, MD, Xi Yang, MD, Bin Tu, MD, Huaping Jia, MD, Qingyi Meng, MD, Jie Liu, MD, Ruizhong Ye, MD
- 2020, 4 (2): 27-42. DOI:10.37015/AUDT.2020.200029
- Abstract ( 1005 ) HTML ( 132 ) PDF ( 8267KB ) ( 682 )
-
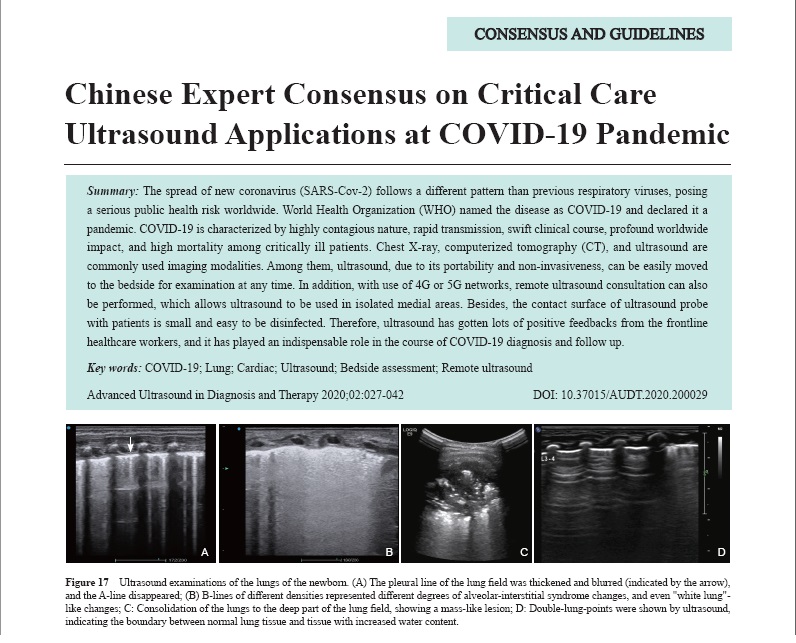
The spread of new coronavirus (SARS-Cov-2) follows a different pattern than previous respiratory viruses, posing a serious public health risk worldwide. World Health Organization (WHO) named the disease as COVID-19 and declared it a pandemic. COVID-19 is characterized by highly contagious nature, rapid transmission, swift clinical course, profound worldwide impact, and high mortality among critically ill patients. Chest X-ray, computerized tomography (CT), and ultrasound are commonly used imaging modalities. Among them, ultrasound, due to its portability and non-invasiveness, can be easily moved to the bedside for examination at any time. In addition, with use of 4G or 5G networks, remote ultrasound consultation can also be performed, which allows ultrasound to be used in isolated medial areas. Besides, the contact surface of ultrasound probe with patients is small and easy to be disinfected. Therefore, ultrasound has gotten lots of positive feedbacks from the frontline healthcare workers, and it has played an indispensable role in the course of COVID-19 diagnosis and follow up.
Review Article
- Critical Care Ultrasonography and Its Application for COVID-19
- Xi Liu, MD, Yang Hai, MD, Bin Ma, MD, Weelic Chong, BA, Ji-Bin Liu, MD
- 2020, 4 (2): 43-49. DOI:10.37015/AUDT.2020.200035
- Abstract ( 965 ) HTML ( 44 ) PDF ( 476KB ) ( 1241 )
-
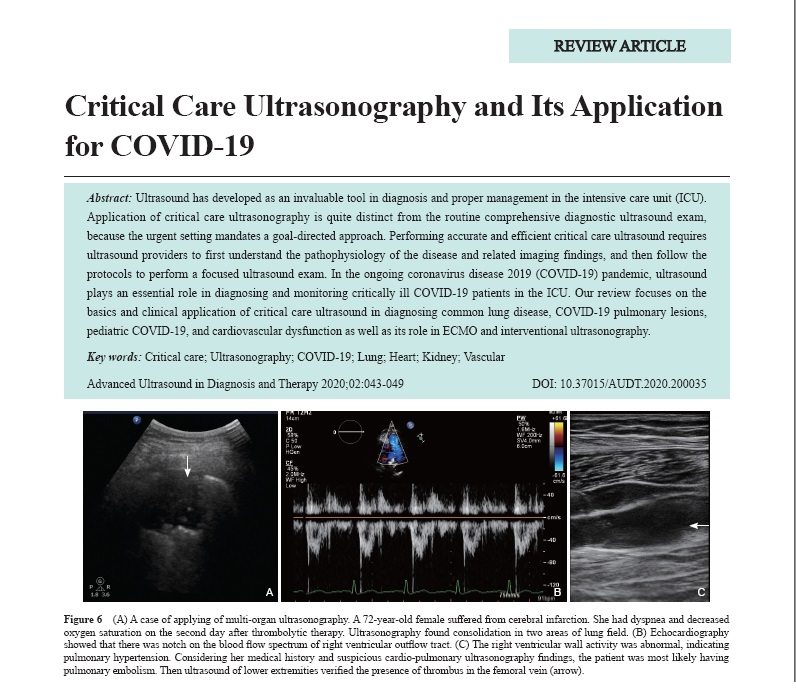
Ultrasound has developed as an invaluable tool in diagnosis and proper management in the intensive care unit (ICU). Application of critical care ultrasonography is quite distinct from the routine comprehensive diagnostic ultrasound exam, because the urgent setting mandates a goal-directed approach. Performing accurate and efficient critical care ultrasound requires ultrasound providers to first understand the pathophysiology of the disease and related imaging findings, and then follow the protocols to perform a focused ultrasound exam. In the ongoing coronavirus disease 2019 (COVID-19) pandemic, ultrasound plays an essential role in diagnosing and monitoring critically ill COVID-19 patients in the ICU. Our review focuses on the basics and clinical application of critical care ultrasound in diagnosing common lung disease, COVID-19 pulmonary lesions, pediatric COVID-19, and cardiovascular dysfunction as well as its role in ECMO and interventional ultrasonography.
- Teleultrasound for the COVID-19 Pandemic: A Statement from China
- Xiaolong Li, MD, Lehang Guo, MD, Liping Sun, MD, PhD. Wenwen Yue, MD, Huixiong Xu, MD, PhD
- 2020, 4 (2): 50-56. DOI:10.37015/AUDT.2020.200036
- Abstract ( 761 ) HTML ( 16 ) PDF ( 612KB ) ( 1019 )
-
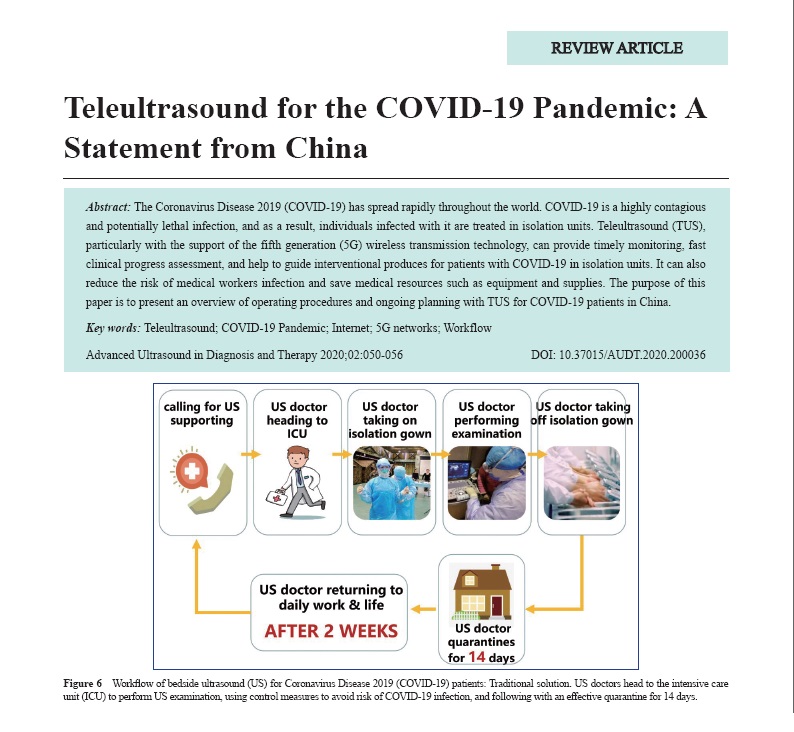
The Coronavirus Disease 2019 (COVID-19) has spread rapidly throughout the world. COVID-19 is a highly contagious and potentially lethal infection, and as a result, individuals infected with it are treated in isolation units. Teleultrasound (TUS), particularly with the support of the fifth generation (5G) wireless transmission technology, can provide timely monitoring, fast clinical progress assessment, and help to guide interventional produces for patients with COVID-19 in isolation units. It can also reduce the risk of medical workers infection and save medical resources such as equipment and supplies. The purpose of this paper is to present an overview of operating procedures and ongoing planning with TUS for COVID-19 patients in China.
- Lung Ultrasonography in Diagnosis and Management of Novel Coronavirus (COVID-19) Pneumonia: Pearls and Pitfalls
- Heng Xue, MD, Yao Zhang, MD, Ligang Cui, MD, Jing Han, MD
- 2020, 4 (2): 57-59. DOI:10.37015/AUDT.2020.200030
- Abstract ( 720 ) HTML ( 14 ) PDF ( 853KB ) ( 756 )
-
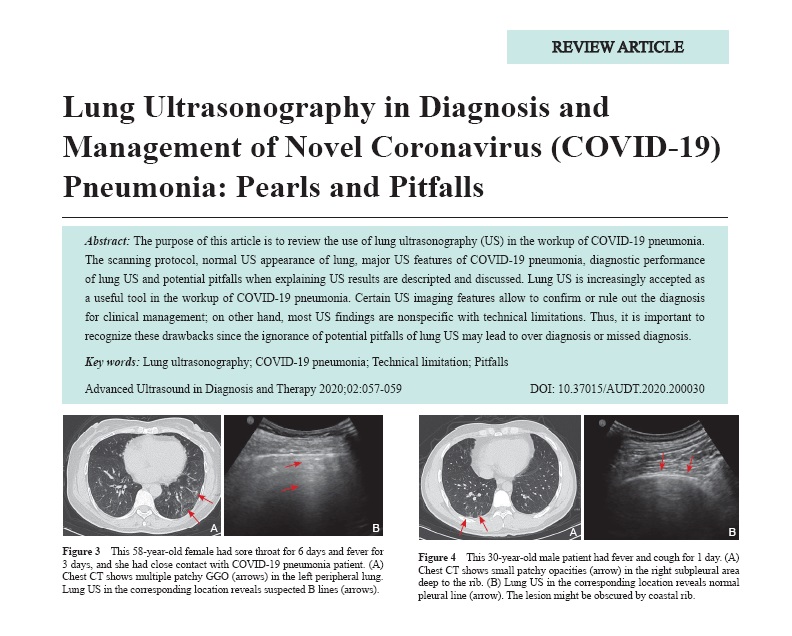
The purpose of this article is to review the use of lung ultrasonography (US) in the workup of COVID-19 pneumonia. The scanning protocol, normal US appearance of lung, major US features of COVID-19 pneumonia, diagnostic performance of lung US and potential pitfalls when explaining US results are descripted and discussed. Lung US is increasingly accepted as a useful tool in the workup of COVID-19 pneumonia. Certain US imaging features allow to confirm or rule out the diagnosis for clinical management; on other hand, most US findings are nonspecific with technical limitations. Thus, it is important to recognize these drawbacks since the ignorance of potential pitfalls of lung US may lead to over diagnosis or missed diagnosis.
Original Research
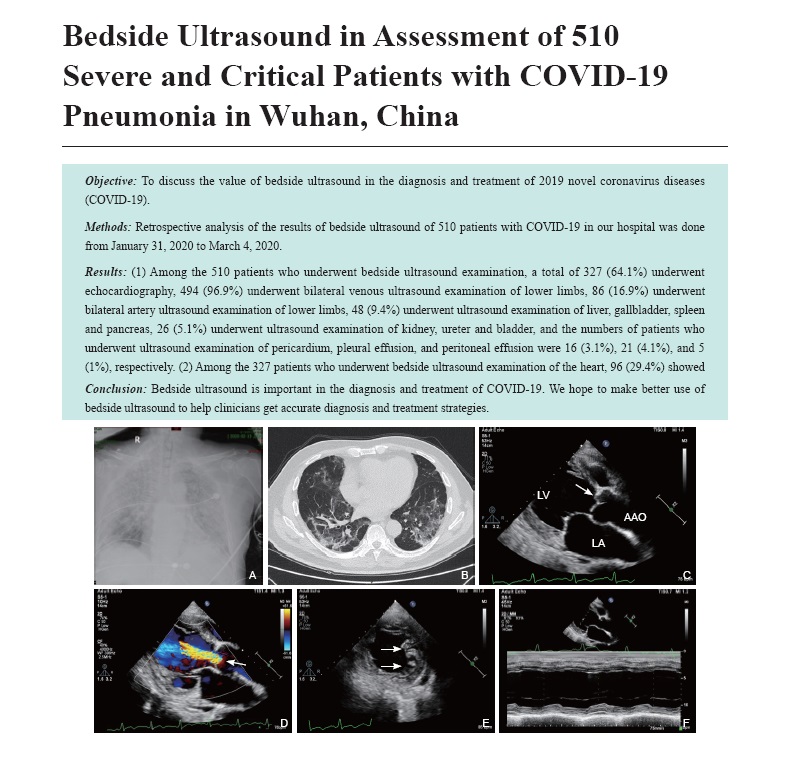
- Bedside Ultrasound in Assessment of 510 Severe and Critical Patients with COVID-19 Pneumonia in Wuhan, China
- Bin Wang, MD, Li Zhang, MD, Danqing Zhang, MD, Hongliang Yuan, MD, Chun Wu, MD, Yongxing Zhang, MD, Lin He, MD, Rui Wang, MD, Jing Wang, MD, Mingxing Xie, MD, PhD
- 2020, 4 (2): 60-66. DOI:10.37015/AUDT.2020.200018
- Abstract ( 559 ) HTML ( 33 ) PDF ( 539KB ) ( 983 )
-
Objective: To discuss the value of bedside ultrasound in the diagnosis and treatment of 2019 novel coronavirus diseases (COVID-19).
Methods: Retrospective analysis of the results of bedside ultrasound of 510 patients with COVID-19 in our hospital was done from January 31, 2020 to March 4, 2020.
Results: (1) Among the 510 patients who underwent bedside ultrasound examination, a total of 327 (64.1%) underwent echocardiography, 494 (96.9%) underwent bilateral venous ultrasound examination of lower limbs, 86 (16.9%) underwent bilateral artery ultrasound examination of lower limbs, 48 (9.4%) underwent ultrasound examination of liver, gallbladder, spleen and pancreas, 26 (5.1%) underwent ultrasound examination of kidney, ureter and bladder, and the numbers of patients who underwent ultrasound examination of pericardium, pleural effusion, and peritoneal effusion were 16 (3.1%), 21 (4.1%), and 5 (1%), respectively. (2) Among the 327 patients who underwent bedside ultrasound examination of the heart, 96 (29.4%) showed results of positive for other abnormalities or complications, in which 31 (9.5%) had abnormal left ventricular wall motion, 42 (12.8%) were with valvular heart disease, 3 (0.9%) showed coronary heart disease, 19 (5.8%) showed the enlargement of right heart with pulmonary hypertension (PAH), and 1 (0.3%) had congenital heart disease. In addition, 6 of the 327 echocardiography patients showed negative results (no other abnormalities or complications), accounting for 1.8%. (3) Among the 494 patients who underwent bilateral venous examination of lower limbs, 182 (36.8%) had phlebothrombosis. Eighty-six (86) patients underwent bilateral artery examination of lower limbs, and 63 (73%) of them had positive results, in which 5 patients showed arterial occlusion and the other 57 patients showed atherosclerosis. (4) Thirty-three (33) patients underwent ultrasound examination of liver, gallbladder, spleen, and pancreas, and 23 (70%) of them showed positive results. Among the 26 patients who underwent the urological examination, 7 (26.9%) showed positive results. Additionally, there are 2 positive findings in 21 patients who underwent the examination of pleural effusion (9.5%), and 1 positive case in 5 patients who underwent the examination of abdominal effusion (20%).
Conclusion: Bedside ultrasound is important in the diagnosis and treatment of COVID-19. We hope to make better use of bedside ultrasound to help clinicians get accurate diagnosis and treatment strategies.
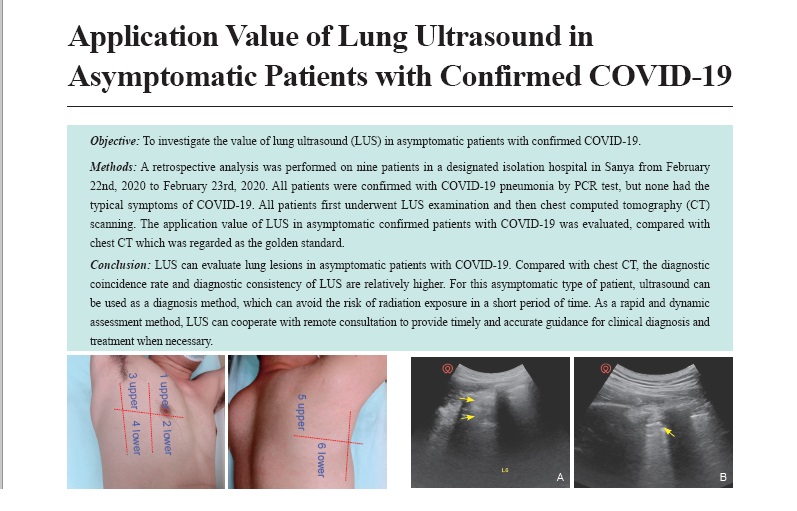
- Application Value of Lung Ultrasound in Asymptomatic Patients with Confirmed COVID-19
- Haidan Lin, MD, Bingqi Zhang, MD, Haiyan Kou, MD, Yuanyuan Zhao, MD, Keyan Li, MD, Dudu Wu, MD, Shiyue Zhao, MD, Liuqiong Ren, MD, Xingxi Lin, MD, Zihao Zhang, MD, Zhiye Chen, MD, Xuexia Shan, MD, Yuqing Huang, MD, Shengzheng Wu, MD, Faqin Lv, MD
- 2020, 4 (2): 67-72. DOI:10.37015/AUDT.2020.200025
- Abstract ( 827 ) HTML ( 31 ) PDF ( 496KB ) ( 1522 )
-
Objective: To investigate the value of lung ultrasound (LUS) in asymptomatic patients with confirmed COVID-19.
Methods: A retrospective analysis was performed on nine patients in a designated isolation hospital in Sanya from February 22nd, 2020 to February 23rd, 2020. All patients were confirmed with COVID-19 pneumonia by PCR test, but none had the typical symptoms of COVID-19. All patients first underwent LUS examination and then chest computed tomography (CT) scanning. The application value of LUS in asymptomatic confirmed patients with COVID-19 was evaluated, compared with chest CT which was regarded as the golden standard.
Results: Among nine asymptomatic patients with COVID-19, there were two cases (22.22%) with abnormal ultrasonic manifestations, of which one (11.11%) showed a fusion B3-line in zone 5 of the right lung, and the other showed localized pulmonary consolidation in zone 6 of the left lung. The remaining seven cases (77.78%) showed no abnormal changes in LUS, but only clear pleura sliding sign and A-line. Chest CT showed abnormal changes in three cases (33.33%). Two of them (22.22%) showed flocculent high-density shadow at the base of both lungs (especially in the right lung), while the other case showed ground-glass opacity with thickened interlobular septal in the left lower lobe, involving the pleura. There were no abnormalities on chest CT of the remaining six cases (66.67%). The two (22.22%) LUS-positive patients were in complete coincidence with CT-positive patients. This study showed that the coincidence rate of the two examination methods was 88.89%. Taking chest CT as golden standard, the sensitivity, specificity, positive predictive value, negative predictive value, and Kappa value of lung ultrasound in the diagnosis of COVID-19 were 66.67%, 100%, 100%, 85.71%, and 0.727, respectively.
Conclusion: LUS can evaluate lung lesions in asymptomatic patients with COVID-19. Compared with chest CT, the diagnostic coincidence rate and diagnostic consistency of LUS are relatively higher. For this asymptomatic type of patient, ultrasound can be used as a diagnosis method, which can avoid the risk of radiation exposure in a short period of time. As a rapid and dynamic assessment method, LUS can cooperate with remote consultation to provide timely and accurate guidance for clinical diagnosis and treatment when necessary.
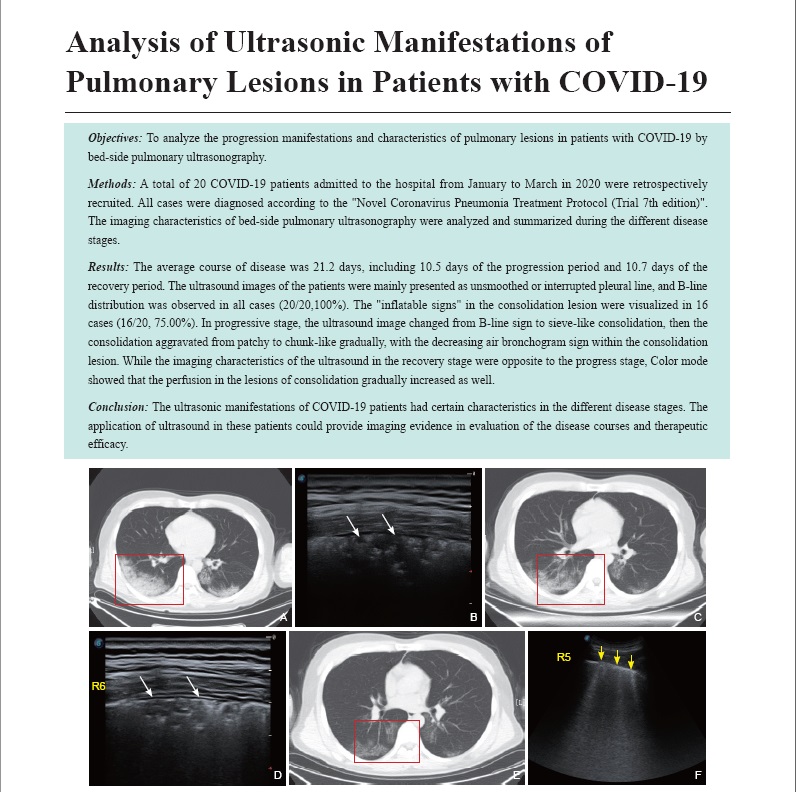
- Analysis of Ultrasonic Manifestations of Pulmonary Lesions in Patients with COVID-19
- Yi Huang, MD, Hua Wang, MD, Wenqi Cui, MD, Yujin Zong, MD, Chuyun Zheng, MD, Yue Liu, MD, Weili Min, MD, Sihan Wang, MD, Mingjun Hu, MD, Yaohui Zhang, MD
- 2020, 4 (2): 73-78. DOI:10.37015/AUDT.2020.200034
- Abstract ( 726 ) HTML ( 20 ) PDF ( 622KB ) ( 804 )
-
Objectives: To analyze the progression manifestations and characteristics of pulmonary lesions in patients with COVID-19 by bed-side pulmonary ultrasonography.
Methods: A total of 20 COVID-19 patients admitted to the hospital from January to March in 2020 were retrospectively recruited. All cases were diagnosed according to the "Novel Coronavirus Pneumonia Treatment Protocol (Trial 7th edition)". The imaging characteristics of bed-side pulmonary ultrasonography were analyzed and summarized during the different disease stages.
Results: The average course of disease was 21.2 days, including 10.5 days of the progression period and 10.7 days of the recovery period. The ultrasound images of the patients were mainly presented as unsmoothed or interrupted pleural line, and B-line distribution was observed in all cases (20/20,100%). The "inflatable signs" in the consolidation lesion were visualized in 16 cases (16/20, 75.00%). In progressive stage, the ultrasound image changed from B-line sign to sieve-like consolidation, then the consolidation aggravated from patchy to chunk-like gradually, with the decreasing air bronchogram sign within the consolidation lesion. While the imaging characteristics of the ultrasound in the recovery stage were opposite to the progress stage, Color mode showed that the perfusion in the lesions of consolidation gradually increased as well.
Conclusion: The ultrasonic manifestations of COVID-19 patients had certain characteristics in the different disease stages. The application of ultrasound in these patients could provide imaging evidence in evaluation of the disease courses and therapeutic efficacy.
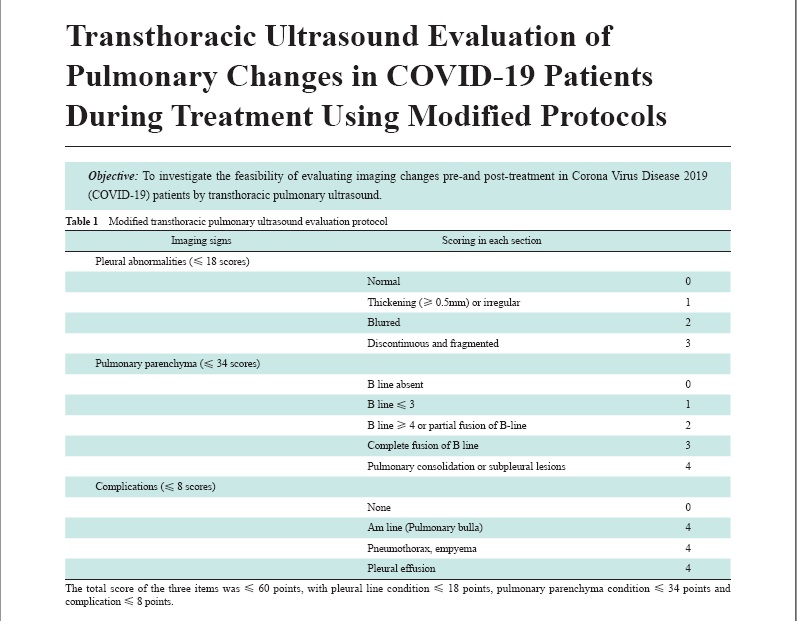
- Transthoracic Ultrasound Evaluation of Pulmonary Changes in COVID-19 Patients During Treatment Using Modified Protocols
- Guorong Lyu, MD, Ying Zhang, MD, Guoliang Tan, MD
- 2020, 4 (2): 79-83. DOI:10.37015/AUDT.2020.200020
- Abstract ( 569 ) HTML ( 17 ) PDF ( 548KB ) ( 729 )
-
Objective: To investigate the feasibility of evaluating imaging changes pre-and post-treatment in Corona Virus Disease 2019 (COVID-19) patients by transthoracic pulmonary ultrasound.
Methods: A total of 8 patients diagnosed with severe or critical COVID-19 pneumonia were recruited, and then ultrasound scanning was performed to evaluate the pulmonary imaging changes pre- and post-treatment based on a modified ultrasonic Buda protocol. The correlation between chest high resolution computed tomography (HRCT) Warrick scoring and ultrasonic results was analyzed.
Results: The main manifestations of ultrasonic imaging in severe or critical COVID-19 patients were: (1) pleural thickening (8/8), blurry or irregular fragmentation (6/8), and discontinuous fragmentation (4/8); (2) pulmonary lesions: B-line sign (2/8), partial or complete fusion of B-line (white lung) (8/8), and pulmonary or subpleural small consolidation (C-line sign) in severe cases (3/8); and (3) rarely, pleural effusion or pulmonary gas cyst (1/8). The imaging results, which were evaluated followed by a modified Buda transthoracic pulmonary ultrasound protocol, were highly correlated with HRCT Warrick scoring (r = 0.715, P < 0.05). Meanwhile, both ultrasonic and HRCT imaging results were significantly improved with progressive COVID-19 treatment (P < 0.05).
Conclusion: The ultrasonic pulmonary imaging of COVID-19 patients manifested several characteristics. The modified Buda transthoracic pulmonary ultrasound protocol could be an alternative method to evaluate the pulmonary lesions in COVID-19 patients.
- Suggestions on Prevention and Control of COVID-19 in Ultrasound Department
- Xuexia Shan, MD, Yuqing Huang, MD, Haiyan Kou, MD, Yuanyuan Zhao, MD, Keyan Li, MD, Dudu Wu, MD, Shiyue Zhao, MD, Liuqiong Ren, MD, Xingxi Lin, MD, Xianghui Chen, MD, Libo Wang, MD, Shengzheng Wu, MD, Faqin Lv, MD
- 2020, 4 (2): 84-89. DOI:10.37015/AUDT.2020.200022
- Abstract ( 439 ) HTML ( 18 ) PDF ( 442KB ) ( 903 )
-
Although the outbreak in China has been effectively controlled, the international situation of prevention and control of coronavirus disease 2019 (COVID-19) still poses a serious public health risk. COVID-19 has been declared a pandemic by World Health Organization (WHO) due to its highly contagious nature, rapid transmission, swift clinical course, profound worldwide impact, and high mortality among critically ill patients. COVID-19 is mainly transmitted by respiratory droplets and contact routes, which could be effectively prevented by proper medical equipment and hand hygiene. However, due to the lack of effective protective measures and personal protective equipment of healthcare personnel in some area, the infectious rate of COVID-19 remains high, especially in clinical settings. At present, due to its portability and accuracy, ultrasound has been playing an indispensable role in the diagnosis, evaluation, and follow-up of COVID-19 patients, especially those in severe conditions. In the course of diagnosis and treatment, because sonographers often work closely with patients, coupled with the increasing number of patients and relatively poor ventilation in the working area, the risk of occupational exposure is undoubtedly high. This article combined the standard precaution methods with current Chinese government's COVID-19 strategy and polices, aiming to provide suggestions on the prevention and control of COVID-19 pandemic for ultrasound professionals.
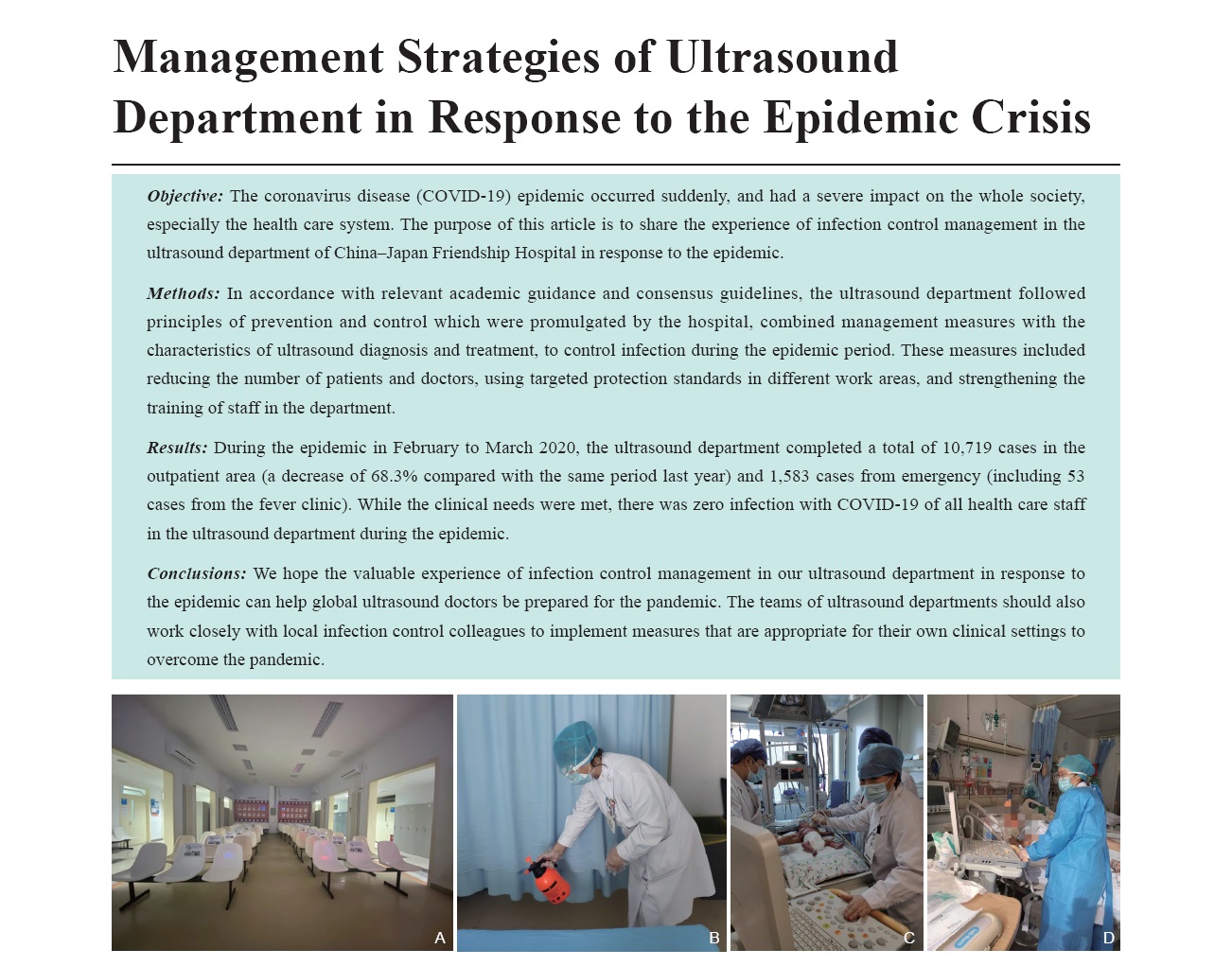
- Management Strategies of Ultrasound Department in Response to the Epidemic Crisis
- Jie Chen, MD, Bo Zhang, MD, Mo Yang, MB, Yan Tian, MD, Dandan Guo, MS, Boya Wang, MD, Weidan Lu, MS, Jiaojiao Ma, MS, Cui Zhao, MB, Shuliang Zang, MB, Jianya Wang, MB
- 2020, 4 (2): 90-98. DOI:10.37015/AUDT.2020.200032
- Abstract ( 576 ) HTML ( 25 ) PDF ( 432KB ) ( 502 )
-
Objective: The coronavirus disease (COVID-19) epidemic occurred suddenly, and had a severe impact on the whole society, especially the health care system. The purpose of this article is to share the experience of infection control management in the ultrasound department of China-Japan Friendship Hospital in response to the epidemic.
Methods: In accordance with relevant academic guidance and consensus guidelines, the ultrasound department followed principles of prevention and control which were promulgated by the hospital, combined management measures with the characteristics of ultrasound diagnosis and treatment, to control infection during the epidemic period. These measures included reducing the number of patients and doctors, using targeted protection standards in different work areas, and strengthening the training of staff in the department.
Results: During the epidemic in February to March 2020, the ultrasound department completed a total of 10,719 cases in the outpatient area (a decrease of 68.3% compared with the same period last year) and 1,583 cases from emergency (including 53 cases from the fever clinic). While the clinical needs were met, there was zero infection with COVID-19 of all health care staff in the ultrasound department during the epidemic.
Conclusions: We hope the valuable experience of infection control management in our ultrasound department in response to the epidemic can help global ultrasound doctors be prepared for the pandemic. The teams of ultrasound departments should also work closely with local infection control colleagues to implement measures that are appropriate for their own clinical settings to overcome the pandemic.
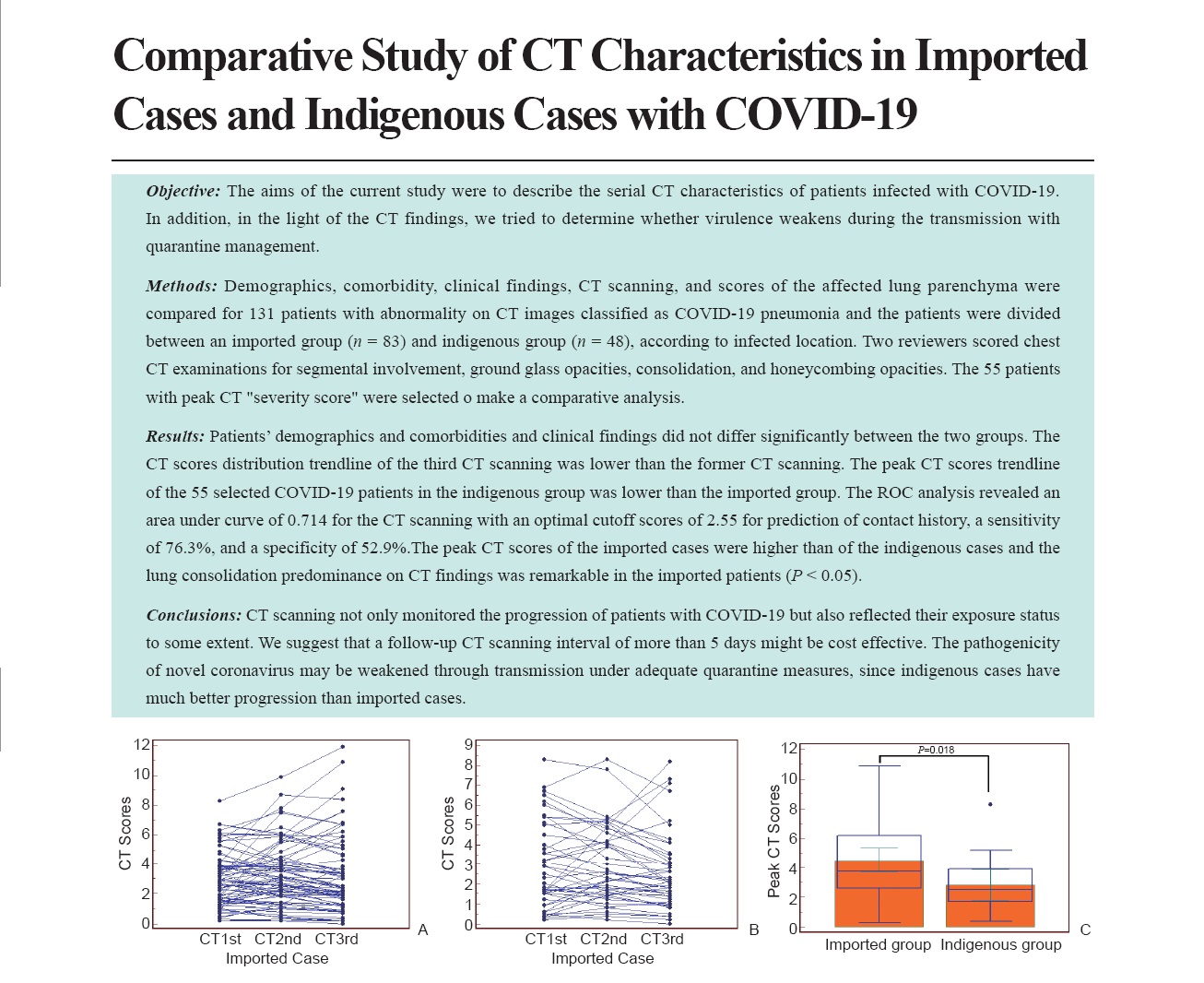
- Comparative Study of CT Characteristics in Imported Cases and Indigenous Cases with COVID-19
- Rong Tan, MD, Nina Li, MD, Ping Liu, MD, Qi Tang, MD, Qizhi Yu, MD
- 2020, 4 (2): 99-106. DOI:10.37015/AUDT.2020.200016
- Abstract ( 667 ) HTML ( 12 ) PDF ( 590KB ) ( 1099 )
-
Objective: The aims of the current study were to describe the serial CT characteristics of patients infected with COVID-19. In addition, in the light of the CT findings, we tried to determine whether virulence weakens during the transmission with quarantine management.
Methods: Demographics, comorbidity, clinical findings, CT scanning, and scores of the affected lung parenchyma were compared for 131 patients with abnormality on CT images classified as COVID-19 pneumonia and the patients were divided between an imported group (n = 83) and indigenous group (n = 48), according to infected location. Two reviewers scored chest CT examinations for segmental involvement, ground glass opacities, consolidation, and honeycombing opacities. The 55 patients with peak CT "severity score" were selected o make a comparative analysis.
Results: Patients’ demographics and comorbidities and clinical findings did not differ significantly between the two groups. The CT scores distribution trendline of the third CT scanning was lower than the former CT scanning. The peak CT scores trendline of the 55 selected COVID-19 patients in the indigenous group was lower than the imported group. The ROC analysis revealed an area under curve of 0.714 for the CT scanning with an optimal cutoff scores of 2.55 for prediction of contact history, a sensitivity of 76.3%, and a specificity of 52.9%.The peak CT scores of the imported cases were higher than of the indigenous cases and the lung consolidation predominance on CT findings was remarkable in the imported patients (P < 0.05).
Conclusions: CT scanning not only monitored the progression of patients with COVID-19 but also reflected their exposure status to some extent. We suggest that a follow-up CT scanning interval of more than 5 days might be cost effective. The pathogenicity of novel coronavirus may be weakened through transmission under adequate quarantine measures, since indigenous cases have much better progression than imported cases.
- Analysis of Characteristics of Bedside Chest Radiography in Critically Ill COVID-19 Patients
- Yijun Zhang, MD, Jianjian Liu, MD, Qinqin Yan, MD, Nannan Shi, MD, Fei Shan, MD, Yuxin Shi, MD
- 2020, 4 (2): 107-111. DOI:10.37015/AUDT.2020.200026
- Abstract ( 415 ) HTML ( 5 ) PDF ( 471KB ) ( 694 )
-
Objective: To analyze the characteristics of bedside chest radiography in critically ill COVID-19 patients.
Methods: Bedside chest x-ray data of 8 severe cases with COVID-19 during hospitalization were collected consecutively. The disease was divided into three stages, including early stage (1-4 days), progression stage (5-10 days), and recovery stage(≥11 days). Two radiologists individually analyzed the chest radiographs by a double-blind method and compared the changes of the distribution, morphology, and boundary of the pulmonary lesions, as well as mediastinum and heart shadow of different disease stages.
Results: Among these cases, 1 case was in the early stage, 6 cases were in the progressive stage, and 1 case was in the recovery stage. A total of 68 bedside chest radiographs were obtained. In early stage, lesions were mainly in the external zone of both lungs with increased lamellar density. In progression stage, the lesions involved multiple pulmonary segments and lobes with extensive infiltrating changes. The heart shadow was mildly to moderately enlarged. In recovery stage, the broad distribution of striated density increased in both lungs, and the heart shadow remained enlarged.
Conclusions: The pulmonary lesions in critically ill COVID-19 patients were characterized by rapid progression, extensive distribution, varied manifestations, and possible concomitant cardiac dilatation. Bedside chest radiograph examination could provide certain significance in the follow-up of critically ill patients.
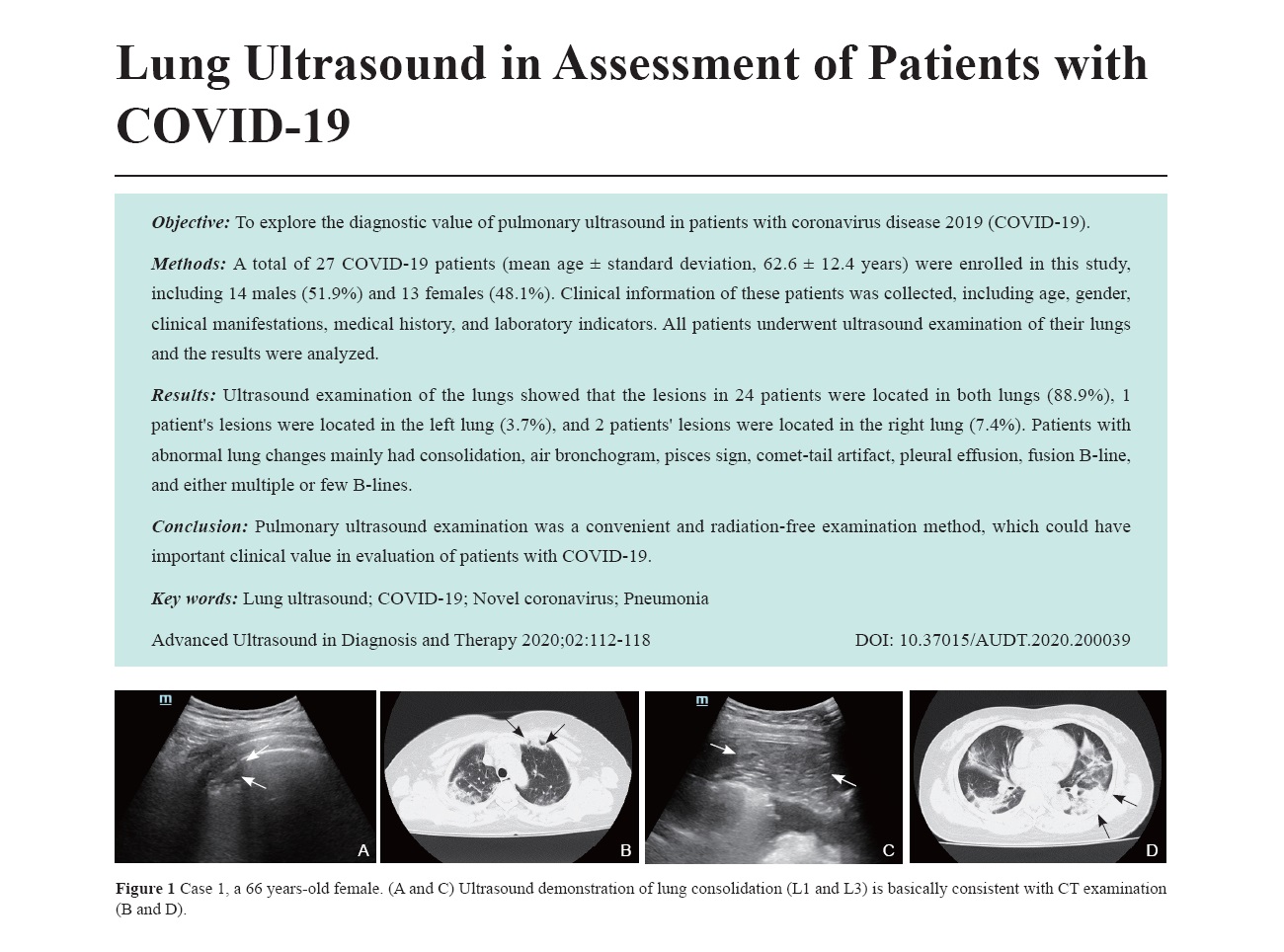
- Lung Ultrasound in Assessment of Patients with COVID-19
- Jianjian Liu, MD, Xin Ma, MD, Xujuan Pu, MD, Jingjing Huang, MD, Zongguo Yang, MD, Xia Shi, MD, Dou Wu, MD, Liping Sun, MD, Hui Zhang, MD
- 2020, 4 (2): 112-118. DOI:10.37015/AUDT.2020.200039
- Abstract ( 460 ) HTML ( 13 ) PDF ( 2195KB ) ( 800 )
-
Objective: To explore the diagnostic value of pulmonary ultrasound in patients with coronavirus disease 2019 (COVID-19).
Methods: A total of 27 COVID-19 patients (mean age ± standard deviation, 62.6 ± 12.4 years) were enrolled in this study, including 14 males (51.9%) and 13 females (48.1%). Clinical information of these patients was collected, including age, gender, clinical manifestations, medical history, and laboratory indicators. All patients underwent ultrasound examination of their lungs and the results were analyzed.
Results: Ultrasound examination of the lungs showed that the lesions in 24 patients were located in both lungs (88.9%), 1 patient's lesions were located in the left lung (3.7%), and 2 patients' lesions were located in the right lung (7.4%). Patients with abnormal lung changes mainly had consolidation, air bronchogram, pisces sign, comet-tail artifact, pleural effusion, fusion B-line, and either multiple or few B-lines.
Conclusion: Pulmonary ultrasound examination was a convenient and radiation-free examination method, which could have important clinical value in evaluation of patients with COVID-19.
Expert Commentary
- Critical Care Ultrasound: A Necessary and Mandatory Tool for Novel Coro-navirus Pneumonia
- Junyu Ma, MD, Xiaoqing Wu, MD, Lina Zhang, MD, Jun Duan, MD, Xiaoting Wang, MD, Chinese Critical Care Ultrasound Study Group (CCUSG)
- 2020, 4 (2): 119-122. DOI:10.37015/AUDT.2020.200040
- Abstract ( 457 ) HTML ( 9 ) PDF ( 461KB ) ( 841 )
-
Ultrasound has developed as an invaluable tool in diagnosis and proper management in the critical care settings. There are four aspects of applying critical care ultrasonography, including substitutional ultrasound, predicational ultrasound, point-of-care ultrasound, and whole body ultrasound. All four aspects have been widely applied in Wuhan based on the special ultrasound lump test predicational critical patients (ULTPCP) protocol. We aim to introduce our own experience of utilizing critical care ultrasound to significantly improve outcomes, shorten the operation time, and reduce occupational exposure.
Case Report
- Application of Remote Ultrasound in COVID-19 Isolated Intensive Care Unit
- Xingxi Lin, MD, Jianqiu Hu, MD, Liuqiong Ren, MD, Yuqing Huang, MD, Dudu Wu, MD, Shiyue Zhao, MD, Yuanyuan Zhao, MD, Jie Liu, MD, Xuan Zhou, MD, Weihua Li, MD, Ming Zhang, MD, Bingqi Zhang, MD, Haidan Lin, MD, Shengzheng Wu, MD, Faqin Lv, MD
- 2020, 4 (2): 123-127. DOI:10.37015/AUDT.2020.200037
- Abstract ( 594 ) HTML ( 16 ) PDF ( 1197KB ) ( 875 )
-
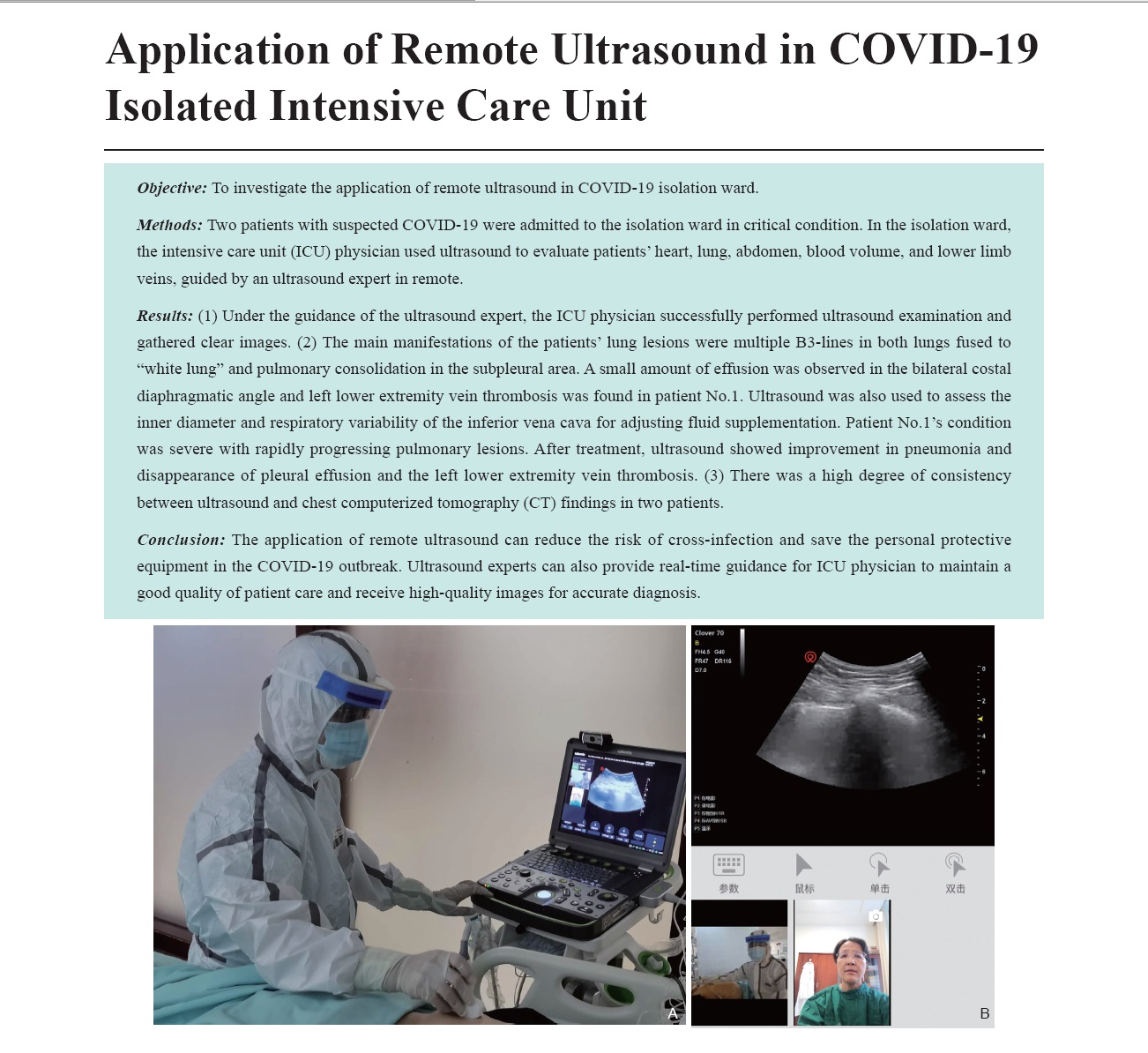
Objective: To investigate the application of remote ultrasound in COVID-19 isolation ward.
Methods: Two patients with suspected COVID-19 were admitted to the isolation ward in critical condition. In the isolation ward, the intensive care unit (ICU) physician used ultrasound to evaluate patients’ heart, lung, abdomen, blood volume, and lower limb veins, guided by an ultrasound expert in remote.
Results: (1) Under the guidance of the ultrasound expert, the ICU physician successfully performed ultrasound examination and gathered clear images. (2) The main manifestations of the patients’ lung lesions were multiple B3-lines in both lungs fused to “white lung” and pulmonary consolidation in the subpleural area. A small amount of effusion was observed in the bilateral costal diaphragmatic angle and left lower extremity vein thrombosis was found in patient No.1. Ultrasound was also used to assess the inner diameter and respiratory variability of the inferior vena cava for adjusting fluid supplementation. Patient No.1’s condition was severe with rapidly progressing pulmonary lesions. After treatment, ultrasound showed improvement in pneumonia and disappearance of pleural effusion and the left lower extremity vein thrombosis. (3) There was a high degree of consistency between ultrasound and chest computerized tomography (CT) findings in two patients.
Conclusion: The application of remote ultrasound can reduce the risk of cross-infection and save the personal protective equipment in the COVID-19 outbreak. Ultrasound experts can also provide real-time guidance for ICU physician to maintain a good quality of patient care and receive high-quality images for accurate diagnosis.
- Robot-assisted Teleultrasound Assessment of Cardiopulmonary Function on a Patient with Confirmed COVID-19 in a Cabin Hospital
- Shengzheng Wu, MD, Keyan Li, MD, Ruizhong Ye, MD, Yuehua Lu, MD, Jufen Xu, MD, Linfei Xiong, MD, Ailin Cui, MD, Yaqing Li, MD, Chengzhong Peng, MD, Faqin Lv, MD
- 2020, 4 (2): 128-130. DOI:10.37015/AUDT.2020.200023
- Abstract ( 859 ) HTML ( 34 ) PDF ( 1578KB ) ( 953 )
-
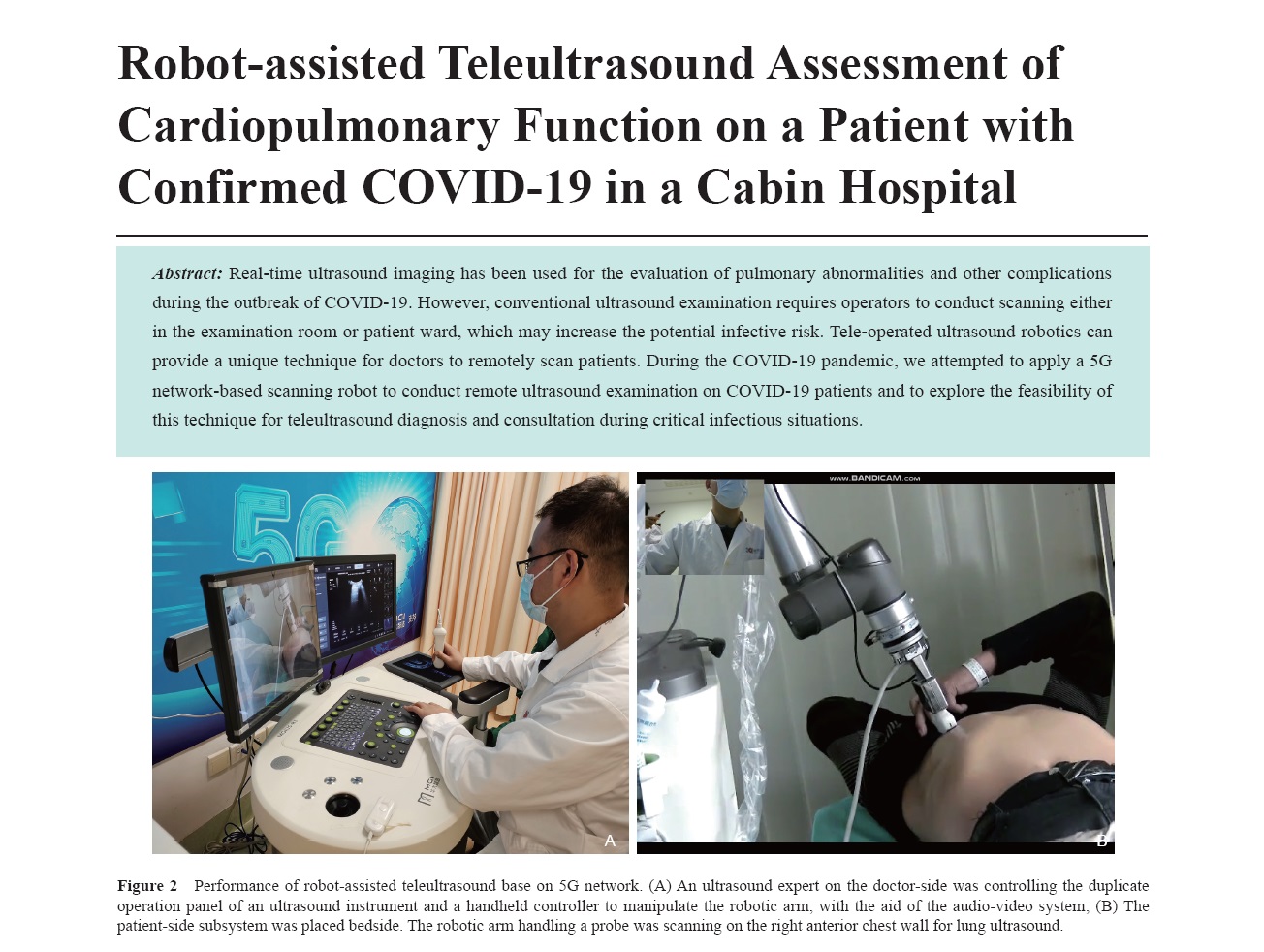
Real-time ultrasound imaging has been used for the evaluation of pulmonary abnormalities and other complications during the outbreak of COVID-19. However, conventional ultrasound examination requires operators to conduct scanning either in the examination room or patient ward, which may increase the potential infective risk. Tele-operated ultrasound robotics can provide a unique technique for doctors to remotely scan patients. During the COVID-19 pandemic, we attempted to apply a 5G network-based scanning robot to conduct remote ultrasound examination on COVID-19 patients and to explore the feasibility of this technique for teleultrasound diagnosis and consultation during critical infectious situations.
- Bedside Ultrasonography-Guided Nasogastric Tube Placement in COVID-19 Patients
- Wenhong Gao, MD, Shunji Gao, MD, Qun-An Huang, MD, Huijuan Xiang, MD
- 2020, 4 (2): 131-133. DOI:10.37015/AUDT.2020.200024
- Abstract ( 683 ) HTML ( 9 ) PDF ( 967KB ) ( 990 )
-
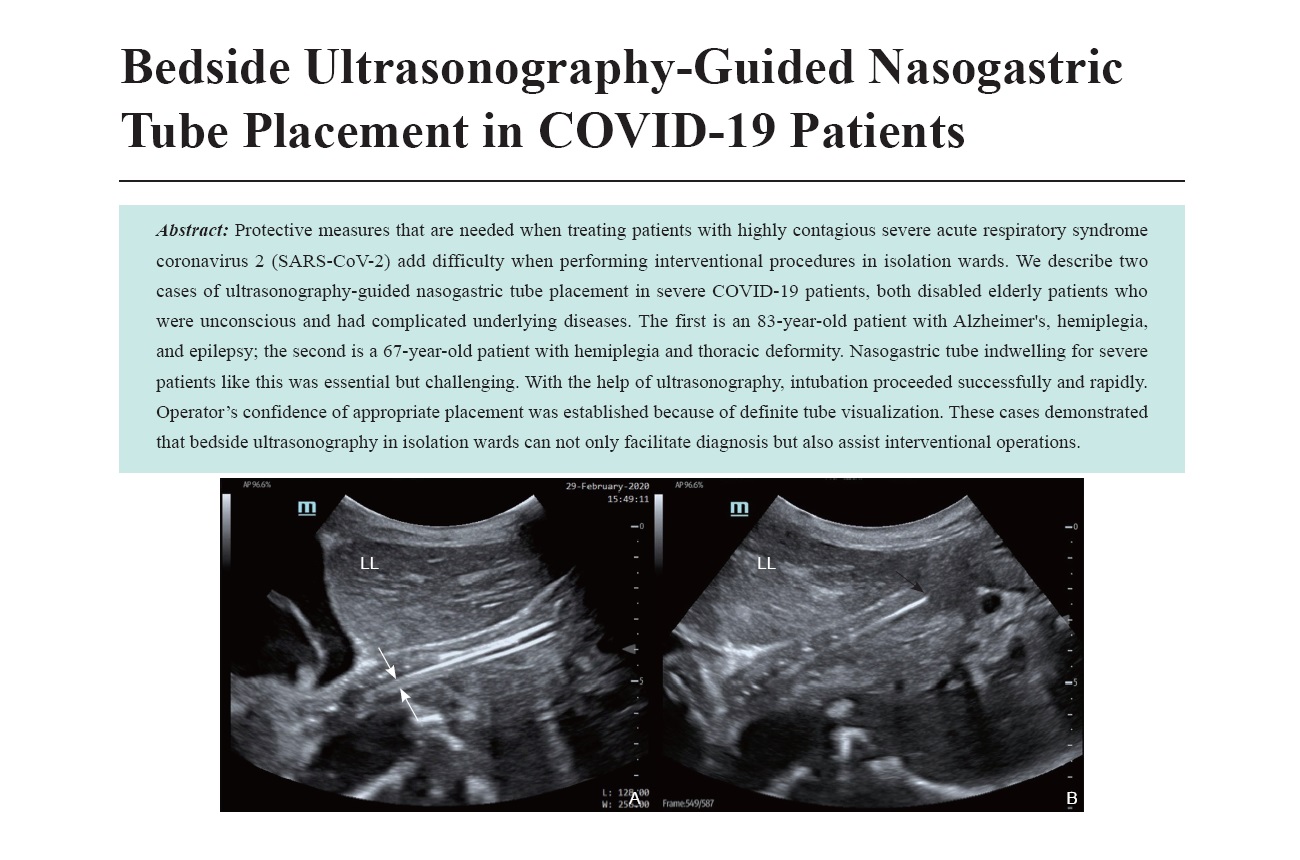
Protective measures that are needed when treating patients with highly contagious severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) add difficulty when performing interventional procedures in isolation wards. We describe two cases of ultrasonography-guided nasogastric tube placement in severe COVID-19 patients, both disabled elderly patients who were unconscious and had complicated underlying diseases. The first is an 83-year-old patient with Alzheimer's, hemiplegia, and epilepsy; the second is a 67-year-old patient with hemiplegia and thoracic deformity. Nasogastric tube indwelling for severe patients like this was essential but challenging. With the help of ultrasonography, intubation proceeded successfully and rapidly. Operator’s confidence of appropriate placement was established because of definite tube visualization. These cases demonstrated that bedside ultrasonography in isolation wards can not only facilitate diagnosis but also assist interventional operations.
- Role of Ultrasound for Management of Critical Severe COVID-19 Patients with ECMO
- Shunji Gao, MD, Liuqiong Ren, MD, Wenhong Gao, MD, Qun’an Huang, MD, Shengzheng Wu, MD, Jianqiu Hu, MD, Yuejuan Gao, MD, Faqin Lv, MD, Huijuan Xiang, MD
- 2020, 4 (2): 134-137. DOI:10.37015/AUDT.2020.200033
- Abstract ( 651 ) HTML ( 13 ) PDF ( 1051KB ) ( 734 )
-
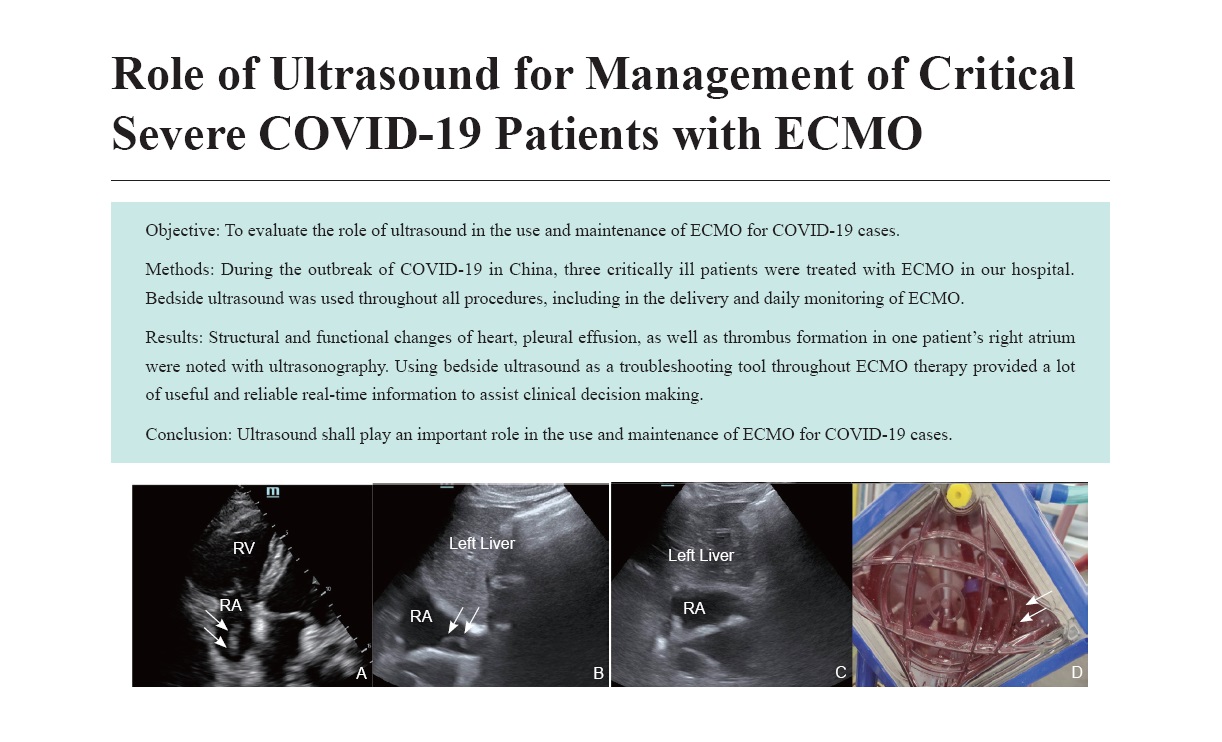
Objective: To evaluate the role of ultrasound in the use and maintenance of ECMO for COVID-19 cases.
Methods: During the outbreak of COVID-19 in China, three critically ill patients were treated with ECMO in our hospital. Bedside ultrasound was used throughout all procedures, including in the delivery and daily monitoring of ECMO.
Results: Structural and functional changes of heart, pleural effusion, as well as thrombus formation in one patient’s right atrium were noted with ultrasonography. Using bedside ultrasound as a troubleshooting tool throughout ECMO therapy provided a lot of useful and reliable real-time information to assist clinical decision making.
Conclusion: Ultrasound shall play an important role in the use and maintenance of ECMO for COVID-19 cases.
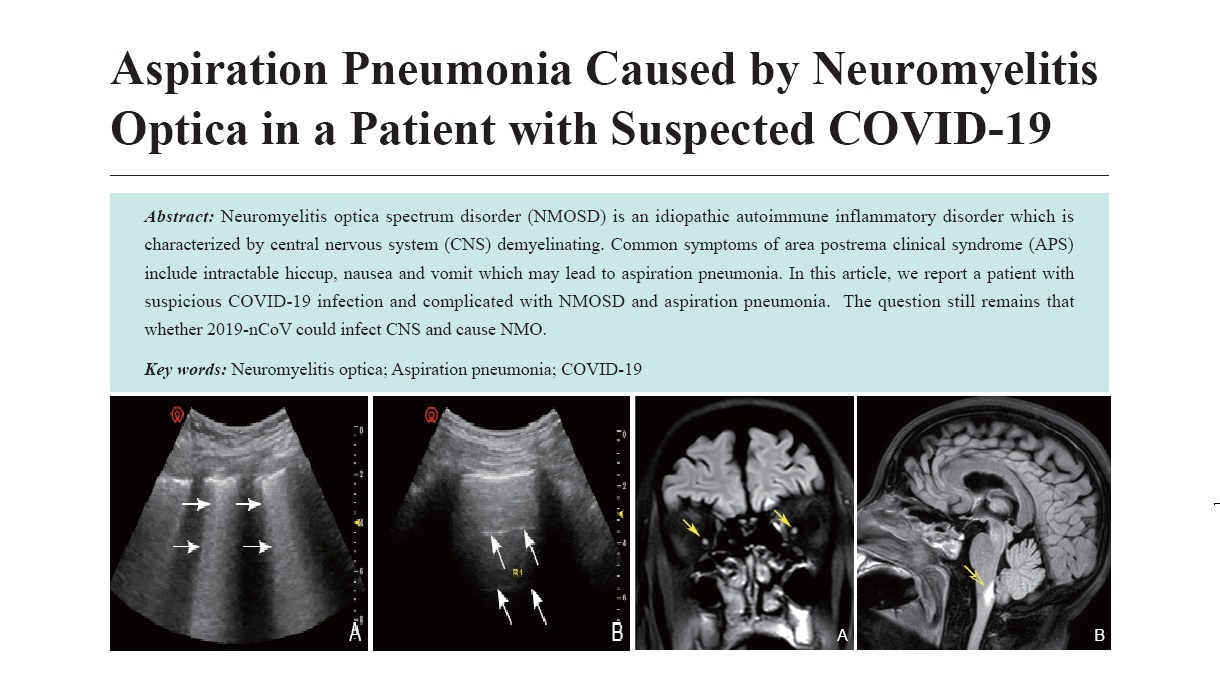
- Aspiration Pneumonia Caused by Neuromyelitis Optica in a Patient with Suspected COVID-19
- Yuanyuan Zhao, MD, Jie Liu, MD, Shengzheng Wu, MD, Weihua Li, MD, Keyan Li, MD, Zhiye Chen, MD, Dudu Wu, MD, Ming Zhang, MD, Ningbo Zhang, MD, Xuan Zhou, Xuexia Shan, Shunji Gao, MD, Faqin Lv, MD
- 2020, 4 (2): 138-141. DOI:10.37015/AUDT.2020.200031
- Abstract ( 601 ) HTML ( 13 ) PDF ( 961KB ) ( 658 )
-
Neuromyelitis optica spectrum disorder (NMOSD) is an idiopathic autoimmune inflammatory disorder which is characterized by central nervous system (CNS) demyelinating. Common symptoms of area postrema clinical syndrome (APS) include intractable hiccup, nausea and vomit which may lead to aspiration pneumonia. In this article, we report a patient with suspicious COVID-19 infection and complicated with NMOSD and aspiration pneumonia. The question still remains that whether 2019-nCoV could infect CNS and cause NMO.
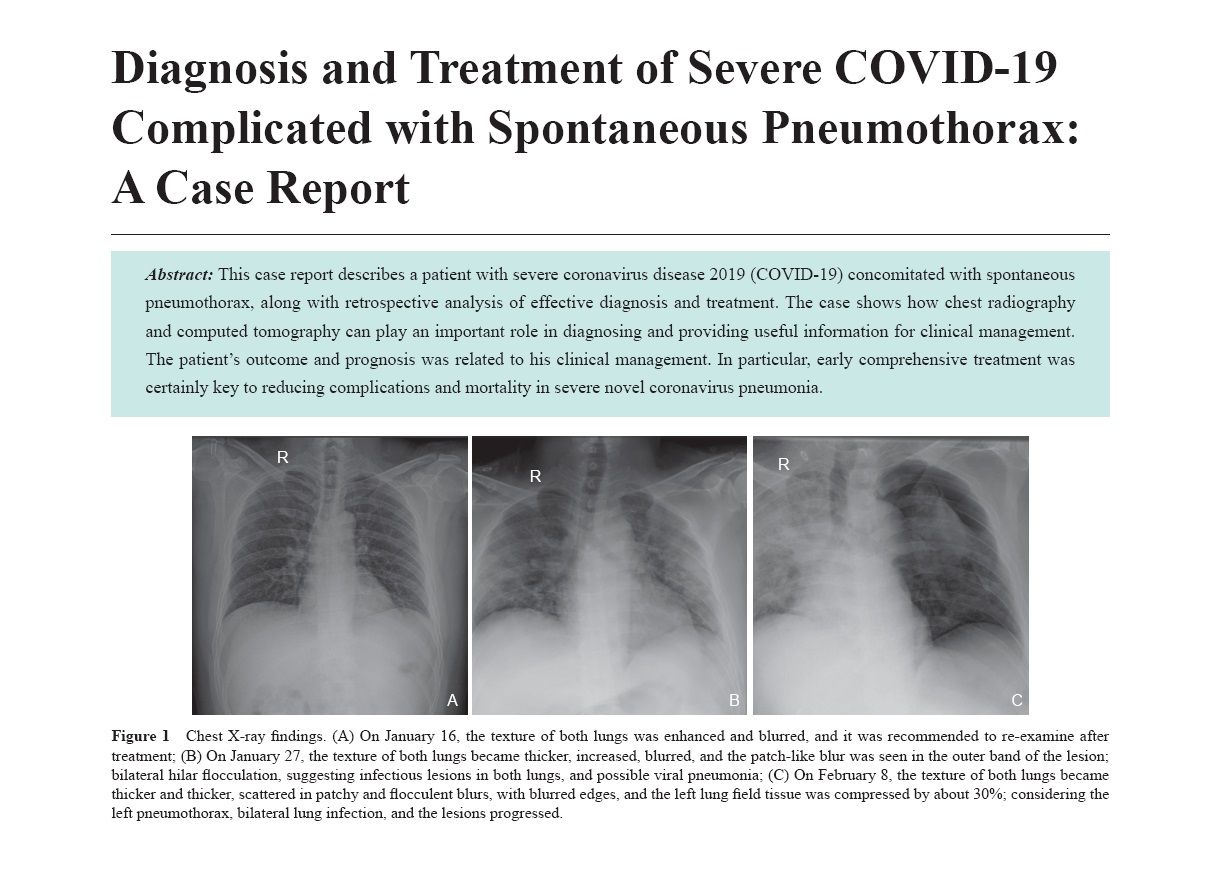
- Diagnosis and Treatment of Severe COVID-19 Complicated with Spontaneous Pneumothorax: A Case Report
- Ruibing Lyu, MD, Xin Li, MD
- 2020, 4 (2): 142-146. DOI:10.37015/AUDT.2020.200019
- Abstract ( 758 ) HTML ( 35 ) PDF ( 1481KB ) ( 952 )
-
This case report describes a patient with severe coronavirus disease 2019 (COVID-19) concomitated with spontaneous pneumothorax, along with retrospective analysis of effective diagnosis and treatment. The case shows how chest radiography and computed tomography can play an important role in diagnosing and providing useful information for clinical management. The patient’s outcome and prognosis was related to his clinical management. In particular, early comprehensive treatment was certainly key to reducing complications and mortality in severe novel coronavirus pneumonia.
Technical Development
- NEW Generation Ultrasound Platform: A Break-through
- Can Huang, MS, Bin Yao, MS, Xixi Zhu, BS, Maolin Ye, MS
- 2020, 4 (2): 147-154.
- Abstract ( 483 ) HTML ( 37 ) PDF ( 3138KB ) ( 570 )
Letter to the Editor
- Point of Care Ultrasound During the Covid-19 Pandemic Should Screen for Inter-Atrial Shunt
- Rajkumar Rajendram, FRCP(Lond), Naveed Mahmood, FRCP(Edin), Ghulam Abbas Kharal, MD, MPH, Mubashar Kharal, MD, Rishi Puri, MBBS, PhD, FRACP
- 2020, 4 (2): 155-156. DOI:10.37015/AUDT.2020.200049
- Abstract ( 397 ) HTML ( 8 ) PDF ( 1351KB ) ( 681 )
Response to Letter
- Reply to Dr. Rajendram’s Letter to Editor: “Point of Care Ultrasound During the Covid-19 Pandemic Should Screen for Inter-Atrial Shunt”
- Xi Liu, MD, Faqin Lv, MD, Ji-Bin Liu, MD
- 2020, 4 (2): 157-158. DOI:10.37015/AUDT.2020.200054
- Abstract ( 312 ) HTML ( 15 ) PDF ( 585KB ) ( 779 )