

ADVANCED ULTRASOUND IN DIAGNOSIS AND THERAPY >
Application Value of Lung Ultrasound in Asymptomatic Patients with Confirmed COVID-19
Received date: 2020-04-01
Online published: 2020-04-17
Objective: To investigate the value of lung ultrasound (LUS) in asymptomatic patients with confirmed COVID-19.
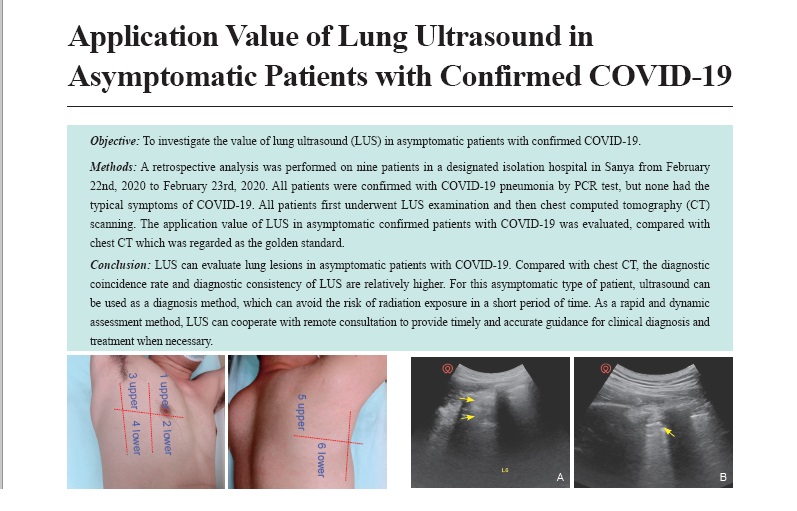
Methods: A retrospective analysis was performed on nine patients in a designated isolation hospital in Sanya from February 22nd, 2020 to February 23rd, 2020. All patients were confirmed with COVID-19 pneumonia by PCR test, but none had the typical symptoms of COVID-19. All patients first underwent LUS examination and then chest computed tomography (CT) scanning. The application value of LUS in asymptomatic confirmed patients with COVID-19 was evaluated, compared with chest CT which was regarded as the golden standard.
Results: Among nine asymptomatic patients with COVID-19, there were two cases (22.22%) with abnormal ultrasonic manifestations, of which one (11.11%) showed a fusion B3-line in zone 5 of the right lung, and the other showed localized pulmonary consolidation in zone 6 of the left lung. The remaining seven cases (77.78%) showed no abnormal changes in LUS, but only clear pleura sliding sign and A-line. Chest CT showed abnormal changes in three cases (33.33%). Two of them (22.22%) showed flocculent high-density shadow at the base of both lungs (especially in the right lung), while the other case showed ground-glass opacity with thickened interlobular septal in the left lower lobe, involving the pleura. There were no abnormalities on chest CT of the remaining six cases (66.67%). The two (22.22%) LUS-positive patients were in complete coincidence with CT-positive patients. This study showed that the coincidence rate of the two examination methods was 88.89%. Taking chest CT as golden standard, the sensitivity, specificity, positive predictive value, negative predictive value, and Kappa value of lung ultrasound in the diagnosis of COVID-19 were 66.67%, 100%, 100%, 85.71%, and 0.727, respectively.
Conclusion: LUS can evaluate lung lesions in asymptomatic patients with COVID-19. Compared with chest CT, the diagnostic coincidence rate and diagnostic consistency of LUS are relatively higher. For this asymptomatic type of patient, ultrasound can be used as a diagnosis method, which can avoid the risk of radiation exposure in a short period of time. As a rapid and dynamic assessment method, LUS can cooperate with remote consultation to provide timely and accurate guidance for clinical diagnosis and treatment when necessary.
Key words: Asymptomatic patients; COVID-19; Pneumonia; Lung ultrasound; CT
Lin, MD Haidan , Zhang, MD Bingqi , Kou, MD Haiyan , Zhao, MD Yuanyuan , Li, MD Keyan , Wu, MD Dudu , Zhao, MD Shiyue , Ren, MD Liuqiong , Lin, MD Xingxi , Zhang, MD Zihao , Chen, MD Zhiye , Shan, MD Xuexia , Huang, MD Yuqing , Wu, MD Shengzheng , Lv, MD Faqin . Application Value of Lung Ultrasound in Asymptomatic Patients with Confirmed COVID-19[J]. ADVANCED ULTRASOUND IN DIAGNOSIS AND THERAPY, 2020 , 4(2) : 67 -72 . DOI: 10.37015/AUDT.2020.200025
| [1] | Zhu N, Zhang DY, Wang WL, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382:727-733. |
| [2] | National Health Commission of the People’s Republic of China. Novel Coronavirus Pneumonia Diagnosis and Treatment Plan (Trial Version 7). [2020-03-03]. [In Chinese] Available from:http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=qkyxlcyjy202002002. |
| [3] | Kanne JP. Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: Key points for the radiologist. Radiology 2020; 200241. |
| [4] | Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 2012; 38:577-591. |
| [5] | Yilmaz HL, ?zkaya AK, Sar? G?kay S, Tolu Kendir ?, ?enol H. Point-of-care lung ultrasound in children with community acquired pneumonia. Am J Emerg Med 2017; 35:964-969. |
| [6] | Yin WH, Wang XT, Liu DW, Zhao YG, Guan XD, Kang Y, et al. Technical specification for clinical application of critical ultrasonography. Chin J Intern Med 2018; 57:397-417. [In Chinese] Available from:http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhnk201806005. |
| [7] | Phelan AL, Katz R, Gostin LO. The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA 2020; 323:709-710. |
| [8] | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497-506. |
| [9] | Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care 2013; 17:R208. |
| [10] | Burnham EL, Hyzy RC, Paine R, Kelly AM, Quint LE, Lynch D, et al. Detection of fibro proliferation by chest high-resolution CT scan in resolving ARDS. Chest 2014; 146:1196-1204. |
| [11] | Bouhemad B, Zhang M, Lu Q, Rouby JJ. Clinical review: Bedside lung ultrasound in critical care practice. Crit Care 2007; 11:205. |
| [12] | Peterson D, Arntfield R. Critical care ultrasonography. Emerg Med Clin North Am 2014; 32:907-926. |
| [13] | Chavez MA, Shams N, Ellington LE, Naithani N, Gilman RH, Steinhoff MC, et al. Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respiratory Research 2014; 15:50. |
| [14] | Stadlerj AM, Andronikous S, Zar HJ. Lung ultrasound for the diagnosis of community-acquired pneumonia in children. Pediatric Radiology 2017; 47:1412-1419. |
| [15] | Alzahrani SA, Al-Salamah MA, Al-Madani WH, Elbarbary MA. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J 2017; 9:6. |
| [16] | Lichtenstein D. BLUE-protocol and FALLS-protocol: Two applications of lung ultrasound in the critically ill. Chest 2015; 147:1659-1670. |
| [17] | Lichtenstein D. Novel approaches to ultrasonography of the lung and pleural space: Where are we now? Breathe (Sheff) 2017; 13:100-111. |
| [18] | Li M, Zhu HM, WANG H, Song J. Progress of clinical application of lung ultrasound in severe diseases. Chin J Hygiene Rescue (Electronic Edition) 2019; 5:110-177. [In Chinese] Available from:http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhwsyjdzzz201902009. |
| [19] | Omran A, Eesai S, Ibrahim M, El-Sharkawy S. Lung ultrasound in diagnosis and follow up of community acquired pneumonia in infants younger than 1-year old. Clin Respir J 2018; 12:2204-2211. |
| [20] | Ianniello S, Piccolo CL, Buquicchio GL, Trinci M, Miele V. First-line diagnosis of pediatric pneumonia in emergency: lung ultrasound (LUS) in addiction to chest-X ray (CXR) and its role in follow-up. Br J Radiol 2016; 89:20150998. |
| [21] | Yan C, Hui R, Lijuan Z, Zhou Y. Lung ultrasound vs chest X-ray in children with suspected pneumonia confirmed by chest computed tomography: A retrospective cohort study. Exp Ther Med 2020; 19:1363-1369. |
| [22] | Chen HY, Yang ZD, Zhang XQ, Chen HB. Comparative study on lung ultrasound and chest CT in diagnosis of severe pneumonia in infants. Journal of Clinical Pulmonary Medicine 2020; 25:11-14. [In Chinese] Available from:http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=lcfkzz202001004. |
| [23] | Bitar ZI, Maadarani OS, El-Shably AM, Al-Ajmi MJ. Diagnostic accuracy of chest ultrasound in patients with pneumonia in the intensive care unit: a single-hospital study. Health Sci Rep 2018; 2:e102. |
| [24] | Xu L, Liu J, Lu M, Yang D, Zheng X. Liver injury during highly pathogenic human coronavirus infections. liver Int 2020. [2020-03-14] [Epub ahead of print] DOI: 10.1111/liv.14435. |
| [25] | Chen L, Liu HG, Liu W, Liu J, Liu K, Shang J, et al. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 2020; 43:203-208. |
| [25] | [In Chinese] |
/
| 〈 |
|
〉 |