

ADVANCED ULTRASOUND IN DIAGNOSIS AND THERAPY >
A Study on Left Atrial Function in Patients with Essential Hypertension Using Four-Dimensional Echocardiography
Received date: 2023-07-09
Accepted date: 2023-10-10
Online published: 2024-07-01
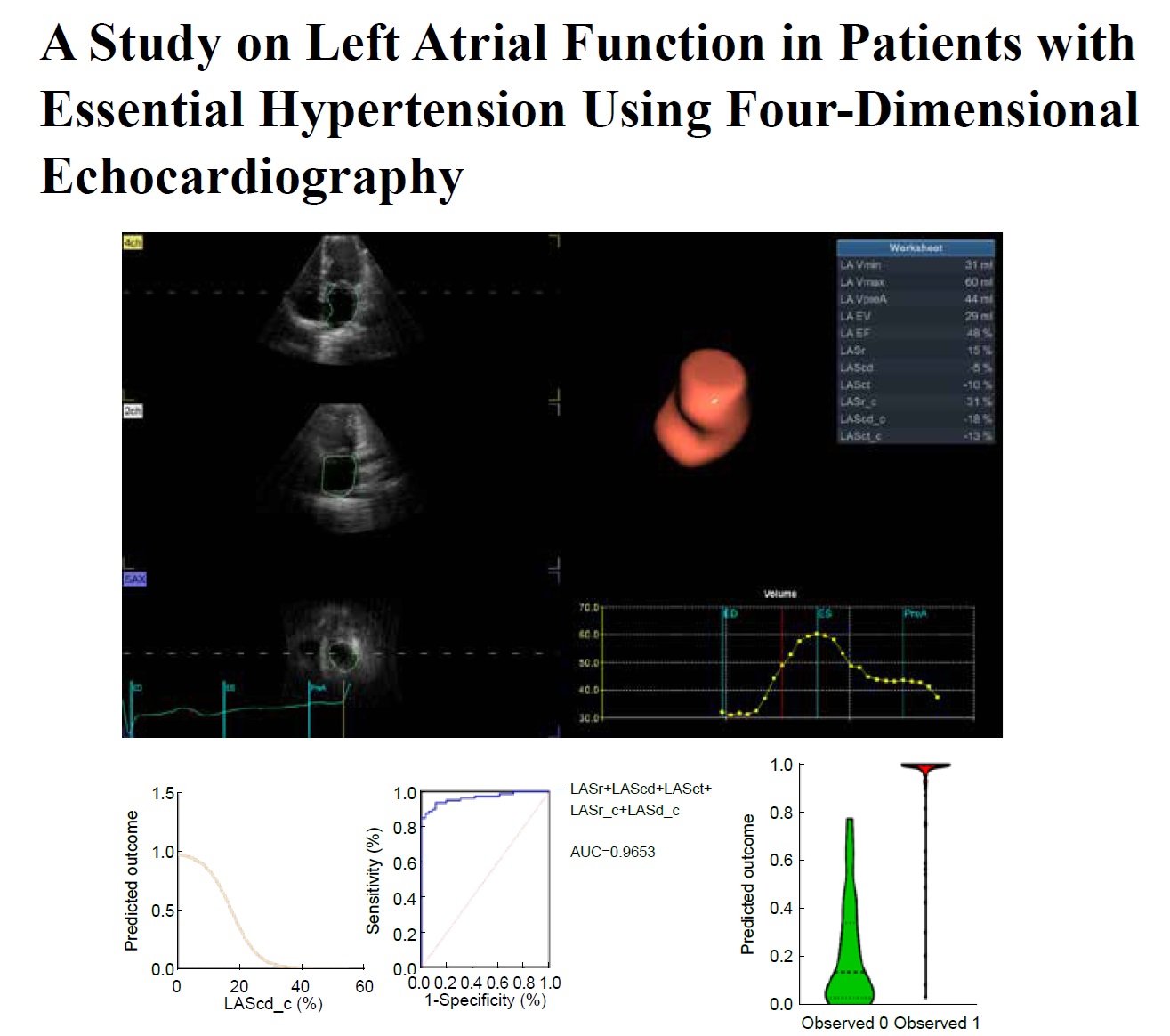
Objective Aimed to evaluate patients with essential hypertension (EH) using four-dimensional automatic left atrial quantification (4DLAQ) To assess the occurrence of EH.
Methods This study selected 80 patients with EH for the EH group and 36 healthy individuals for the control group. Various cardiac parameters, including left atrial diameter (LAD), interventricular septal thickness (IVST), left ventricular end-diastolic diameter (LVDD), left ventricular posterior wall thickness (LVPWT), early E-wave velocity of mitral valve diastole/mitral valve ring myocardial displacement velocity (E/e'), biplanar left ventricular ejection fraction (biplanLVEF), left atrial minimum volume (LAVmin), lateral left atrial maximum volume (LAVmax), left atrial presystolic volume (LAVpreA), left atrial ejection fraction obtained by two-dimensional echocardiography (LAEF), left atrial passive ejection fraction (LAPEF), left atrial active ejection fraction (LAAEF), left atrial reservoir longitudinal strain (LASr), left atrial catheter longitudinal strain (LAScd), left atrial systolic longitudinal strain (LASct), left atrial reservoir circular strain (LASr_c), left atrial catheter circular strain (LAScd_c), and left atrial systolic circular strain (LASct_c) were measured using 4DLAQ. Binary logistic regression was employed to analyze the effect of 4DLAQ strain parameters on EH. Receiver operating characteristic (ROC) curves were used to assess the predictive value of 4DLAQ strain parameters for EH.
Results Systolic blood pressure and diastolic blood pressure in the EH group were higher than those in the control group (P = 0.000 and 0.000, respectively). In the EH group, LAD, IVST, LVDD, LVPWT, E/e', LAVmin, LAVmax, and LAVpreA were significantly increased (P = 0.000, 0.000, 0.072, 0.000, 0.000, 0.001, 0.052, and 0.004, respectively), whereas biplanLVEF, LAEF, LAPEF, LAAEF, LASr, LAScd, LASct, LASr_c, LAScd_c, and LASct_c significantly decreased (P = 0.090, 0.000, 0.009, 0.064, 0.000, 0.000, 0.000, 0.000, 0.000, and 0.689, respectively). Bland-Altman plots were used to illustrate the relationship between variables and audience consensus. LASr and LAScd were identified as independent risk factors for EH. The area under the ROC curve (AUC) for LASr was 0.925, (95% confidence interval [CI] = 0.879-0.971) with a sensitivity of 80.00%, specificity of 94.44%, using a cut-off value of 20%. For LAScd, the AUC-ROC was 0.878 (95% CI = 0.818-0.939 with a sensitivity of 76.25%, specificity 86.11%, and using a critical value of -11%.
Conclusion LASr and LAScd exhibited superior predictive capabilities for EH, with LASr performing the best. This study fills a critical gap in left atrial research and holds significant clinical implications.
Junrong Hong, MD , Pingyang Zhang, MD, PhD , Mengyao Fei, MD , Lingling Wang, MD . A Study on Left Atrial Function in Patients with Essential Hypertension Using Four-Dimensional Echocardiography[J]. ADVANCED ULTRASOUND IN DIAGNOSIS AND THERAPY, 2024 , 8(2) : 64 -73 . DOI: 10.37015/AUDT.2024.230042
| [1] | Zhang GZ, He YB, Huang JY, and Cui JJ. Effect of hypertension on left atrial structure of heart. Journal of Hypertension 1999:219. |
| [2] | Overvad TF, Nielsen PB, Larsen TB, and S?gaard P. Left atrial size and risk of stroke in patients in sinus rhythm. A systematic review. Thromb Haemost 2016; 116:206-219. |
| [3] | Luigi PB, Marcelo HM, Sorina M, Diletta P, Jola X, Martina PM, et al. Left atrial volumes and function by three-dimensional echocardiography: reference values, accuracy, reproducibility, and comparison with two-dimensional echocardiographic measurements. Circ Cardiovasc Imaging 2016; 9:e004229. |
| [4] | Committee of Guidelines for Ambulatory Blood Pressure Monitoring of China Hypertension Alliance. Guidelines for Ambulatory Blood Pressure Monitoring in China in 2020. Chinese Journal of Medical Frontiers (Electronic Edition) 2021; 13:34-51. |
| [5] | Liu HH, Tian GX, and Lin Y. Recognition of atrial function. Chinese Journal of Evidence based Cardiovascular Medicine 2020; 12:1153-1155. |
| [6] | Ahmet K, Cennet Y, Abdülmelik Y, Yavuz K, Metin ?, Ibrahim R, et al. Early detection strain/strain rate and time to strain/strain rate abnormalities for left atrial mechanical function in hypertensive patients. Acta Cardiol 2019; 74:141-151. |
| [7] | Alberto M, Elisabetta P, Corrado M, Diego N, Sara A, Eleonora A, et al. Left atrial enlargement in essential hypertension:role in the assessment of subclinical hypertensive heart disease. Blood Press 2012; 21:88-96. |
| [8] | Wang LL, Zhang PY, Dong J, Ma XW, Ran H, Li L, et al. Assessment of left atrial function in patients with primary hypertension with left ventricular remodeling based on color Doppler ultrasound four-dimensional volume strain technology. Shandong Medical Journal 2021; 61:53-56. |
| [9] | Peng HB, Wang CM, Wang XL, Zhang YT, Li ZL. Clinical study on the evaluation of early left atrial function in patients with essential hypertension using 2D STI technology. Systems Medicine 2019; 4:107-110. |
| [10] | Ran H, Schneider M, Wan LL, Ren JY, Ma XW, Zhang PY. Four-dimensional volume-strain expression in asymptomatic primary hypertension patients presenting with subclinical left atrium-ventricle dysfunction. Cardiology 2020; 145:578-588. |
| [11] | Yoshie I, Satoshi Y, Naoko K, Akiyoshi H, Kikuya U, Tomoaki N, et al. Strain rate imaging for noninvasive functional quantification of the left atrium: comparative studies in controls and patients with atrial fibrillation. J Am Soc Echocardiogr 2005; 18:729-736. |
| [12] | Axel CC, Toralph R, Johan S, Erik I, Anders L, Lars L, et al. Association between circulating endostatin, hypertension duration, and hypertensive target-organ damage. Hypertension 2013; 62:1146-1151. |
| [13] | Daniel AM, Evgeny B, Radhakrishnan AK, Martin K, Athanasios F, Kerstin B, et al. Potential usefulness and clinical relevance of adding left atrial strain to left atrial volume index in the detection of left ventricular diastolic dysfunction. JACC Cardiovasc Imaging 2018; 11:1405-1415. |
| [14] | Thomas L, Marwick TH, Popescu BA, Donal E, and Badano LP. Left atrial structure and function, and left ventricular diastolic dysfunction: JACC State-of-the-Art Review. J Am Coll Cardiol 2019; 73:1961-1977. |
| [15] | Matteo C, Marco MC, Maria M, Pietro A M, Maria L M, Pietro S, et al. Speckle tracking analysis: a new tool for left atrial function analysis in systemic hypertension: an overview. J Cardiovasc Med (Hagerstown) 2016; 17:339-343. |
| [16] | Hirokazu M, Yoshifumi O, Yukio M, Arata I, Norio N, Nusrat A, et al. Effect of an increase in left ventricular pressure overload on left atrial-left ventricular coupling in patients with hypertension: a two-dimensional speckle tracking echocardiographic study. Echocardiography 2013; 30:658-666. |
| [17] | Cesare C, Marijana T, Elisa G, Carla S, Guido G. Targeting subclinical organ damage in obstructive sleep apnea: a narrative review. J Hum Hypertens 2021; 35:26-36. |
| [18] | Zhang R, Zhu HZ, Huang DQ, Zhao QQ, Wang SJ, Wang Y, et al. Application value of four-dimensional automatic left atrial quantitative analysis technology in evaluating left atrial function in patients with essential hypertension. Chinese Journal of Ultrasound Imaging 2021; 30:655-660. |
| [19] | Liu HL, Song Y, and Zhang F. Study on the synchronization of coronary heart disease by three-dimensional speckle tracking technology and real-time three-dimensional echocardiography. China Medical Innovation 2019; 16:10-14. |
| [20] | Fei MY, Li M, Ran H, Sheng ZX, Dong J, and Zhang PY. Four-dimensional quantification on left atrial volume-strain in coronary heart disease patients without regional wall motion abnormalities: Correlation with the severity of coronary stenosis. Echocardiography 2022; 39:758-767. |
| [21] | Chen LL, Zhang CQ, Wang JT, Guo LY, Wang XL, Liu FZ, et al. Left atrial strain measured by 4D Auto LAQ echocardiography is significantly correlated with high risk of thromboembolism in patients with non-valvular atrial fibrillation. Quant Imaging Med Surg 2021; 11:3920-3931. |
/
| 〈 |
|
〉 |