

ADVANCED ULTRASOUND IN DIAGNOSIS AND THERAPY >
Role of Lung Ultrasound in Diagnosing and Differentiating Transient Tachypnea of Newborn and Respiratory Distress Syndrome in Preterm Neonates
Received date: 2021-11-01
Revised date: 2021-11-22
Online published: 2022-08-08
Objective: Transient tachypnea of newborn (TTN) and respiratory distress syndrome (RDS) are the most common causes of respiratory distress among preterm neonates. The aim of this study was to evaluate the accuracy of lung ultrasonography (LUS) for diagnosing and differentiating TTN and RDS in preterm neonates.
Methods: This was a prospective single center study. From January 2020 to June 2021 a total of 114 preterm neonates who were admitted to neonatal intensive care unit (NICU) with symptoms of respiratory distress within 6 hours of birth were subjected to clinical examination, laboratory testing, chest x-ray (AP and lateral view’s) and LUS. Their clinical course was closely monitored. On the basis of final diagnosis made on day three of admission they were divided into two groups, 37 diagnosed with TTN and 61 with RDS. Patients diagnosed with other conditions including neonatal pneumonia, meconium aspiration syndrome etc. were excluded from analysis. LUS findings in RDS and TTN were analyzed and compared to each other.
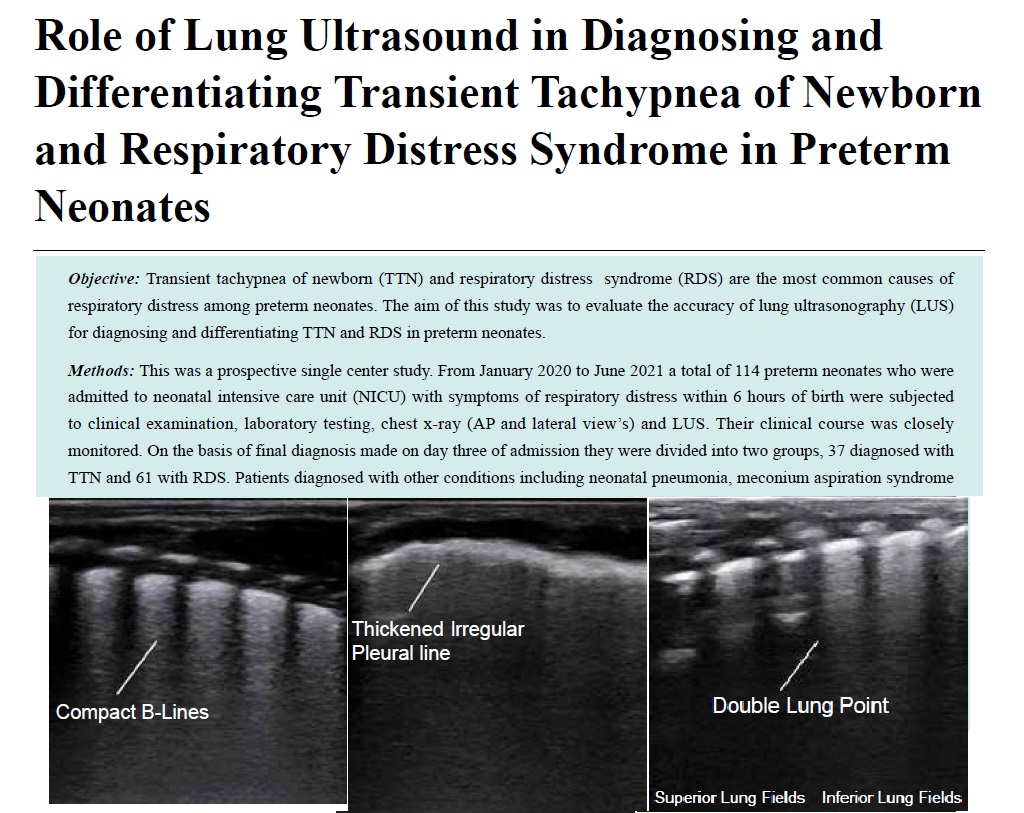
Results: Pulmonary edema manifesting as alveolo-interstitial syndrome, double lung point and less commonly as white out lungs in absence of consolidation had a 100% sensitivity and specificity in diagnosing TTN. A combination of three signs of consolidation with air or fluid bronchograms, white out lungs and absent spared areas has a 100% sensitivity and specificity for diagnosing RDS. Double lung point was seen only in infants suffering from TTN while consolidation with air or fluid bronchograms was only seen in cases of RDS.
Conclusion: Lung ultrasound can accurately diagnose and reliably differentiate TTN and RDS in preterm neonates. Hence LUS can become an initial screening tool in NICU.
S, MD Srinivasan , Aggarwal, MD Neeti , Makhaik, MD Sushma , Jhobta, MD Anupam . Role of Lung Ultrasound in Diagnosing and Differentiating Transient Tachypnea of Newborn and Respiratory Distress Syndrome in Preterm Neonates[J]. ADVANCED ULTRASOUND IN DIAGNOSIS AND THERAPY, 2022 , 6(3) : 112 -118 . DOI: 10.37015/AUDT.2022.210034
| [1] | Estimates developed by the UN Inter-agency Group for Child Mortality Estimation (UNICEF, WHO, World Bank, UN DESA Population Division at childmortality.org. Website. . https://data.worldbank.org/. |
| [2] | Consortium on Safe Labor, Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S, et al. Respiratory morbidity in late preterm births. JAMA. 2010; 304: 419-425. |
| [3] | Mahoney AD, Jain L. Respiratory disorders in moderately preterm, late preterm, and early term infants. Clin Perinatol 2013; 40: 665-678. |
| [4] | Greenough A. Greenough A, Milner AD. Transient tachypnea of the newborn. Neonatal respiratory disorder 2nd ed. London: CRC Press; 2003. 272-277. |
| [5] | Yurdakök M. Transient tachypnea of the newborn: what is new? J Matern Fetal Neonatal Med 2010; 23 Suppl 3: 24-26. |
| [6] | Morris Susan J. Radiology of the chest in neonates. Curr Paediatr 2003; 13:460-468. |
| [7] | Lovrenski J. Lung ultrasonography of pulmonary complications in preterm infants with respiratory distress syndrome. Ups J Med Sci 2012; 117: 10-17. |
| [8] | Mactier H, Bates SE, Johnston T, Lee-Davey C, Marlow N, Mulley K, et al. Perinatal management of extreme preterm birth before 27 weeks of gestation: a framework for practice. Arch Dis Child Fetal Neonatal Ed 2020; 105: 232-239. |
| [9] | Wang J, Liu X, Zhu T, Yan C. Analysis of neonatal respiratory distress syndrome among different gestational segments. Int J Clin Exp Med 2015; 8: 16273-16279. |
| [10] | Rocha G, Rodrigues M, Guimarães H. Respiratory distress syndrome of the preterm neonate--placenta and necropsy as witnesses. J Matern Fetal Neonatal Med 2011; 24: 148-151. |
| [11] | Staub NC. Pulmonary edema. Physiol Rev 1974; 54: 678-811. |
| [12] | Kurl S, Heinonen KM, Kiekara O. The first chest radiograph in neonates exhibiting respiratory distress at birth. Clin Pediatr (Phila) 1997; 36: 285-289. |
| [13] | Copetti R, Cattarossi L, Macagno F, Violino M, Furlan R. Lung ultrasound in respiratory distress syndrome: a useful tool for early diagnosis. Neonatology 2008; 94: 52-59. |
| [14] | Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology: the impact of new epidemiological data. Br J Radiol 2012; 85: e1316-1317. |
| [15] | Raimondi F, Migliaro F, Sodano A, Vallone G, Capasso L. Point-of care chest ultrasound in the neonatal intensive care unit. J Pediatr Neonatal Individual Med 2013; 2: 387-407. |
| [16] | Liu J, Cao HY, Wang XL, Xiao LJ. The significance and the necessity of routinely performing lung ultrasound in the neonatal intensive care units. J Matern Fetal Neonatal Med 2016; 29: 4025-4030. |
| [17] | Chen SW, Fu W, Liu J, Wang Y. Routine application of lung ultrasonography in the neonatal intensive care unit. Medicine (Baltimore) 2017; 96: e5826. |
| [18] | Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O. The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 1997; 156: 1640-1646. |
| [19] | Lichtenstein D, Mezière G. A lung ultrasound sign allowing bedside distinction between pulmonary edema and COPD: the comet-tail artifact. Intensive Care Med 1998; 24: 1331-1334. |
| [20] | Koenig SJ, Narasimhan M, Mayo PH. Thoracic ultrasonography for the pulmonary specialist. Chest 2011; 140: 1332-1341. |
| [21] | Lichtenstein DA, Lascols N, Mezière G, Gepner A. Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med 2004; 30: 276-281. |
| [22] | Lichtenstein D.(2005). Lung ultrasound in the critically ill. Clinical Intensive Care. |
| [23] | Expert Review of Respiratory Medicine 2014, 16, 79-87. |
| [24] | Liu S, Tong X. The clinical comparative study of preterm respiratory distress syndrome and transient tachypnea of newborn. Zhonghua Er Ke Za Zhi 2015; 53: 104-108. [In Chinese] |
| [25] | Mlay GS, Manji KP. Respiratory distress syndrome among neonates admitted at Muhimbili Medical Centre, Dar es Salaam, Tanzania. J Trop Pediatr 2000; 46: 303-307. |
| [26] | Costa S, Rocha G, Leitão A, Guimarães H. Transient tachypnea of the newborn and congenital pneumonia: a comparative study. J Matern Fetal Neonatal Med 2012; 25: 992-994. |
| [27] | Levine EM, Ghai V, Barton JJ, Strom CM. Mode of delivery and risk of respiratory diseases in newborns. Obstet Gynecol 2001; 97: 439-442. |
| [28] | Chandrasekhar R, Manchu M and Vijaya L. Clinical study of respiratory distress in new born. International Journal of Contemporary Pediatrics 2016; 3: 910-915. |
| [29] | Miserocchi G: The interstitial and microvascular unit of the lung: from the neonate to the adult; in Weir EK, Reeves JT, Reeves Sl (eds): Pulmonary Edema. Oxford, Futura (Blackwell), 1998. |
/
| 〈 |
|
〉 |