| [1] |
Neumann E, Rosenheck K. Permeability changes induced by electric impulses in vesicular membranes. J Membrane Biol 1972; 10: 279-290.
|
| [2] |
Zimmermann U. Electric field-mediated fusion and related electrical phenomena. Biochim Biophys Acta 1982; 694: 227-277.
|
| [3] |
Weaver JC. Electroporation: a general phenomenon for manipulating cells and tissues. J Cell Biochem 1993; 51: 426-435.
|
| [4] |
Freeman SA, Wang MA, Weaver JC. Theory of electroporation of planar bilayer membranes: predictions of the aqueous area, change in capacitance, and pore-pore separation. Biophys J 1994; 67: 42-56.
|
| [5] |
Geboers B, Scheffer HJ, Graybill PM, Ruarus AH, Nieuwenhuizen S, Puijk RS, et al. High-voltage electrical pulses in oncology: irreversible electroporation, electrochemotherapy, gene electrotransfer, electrofusion, and electroimmunotherapy. Radiology 2020; 295: 254-272.
|
| [6] |
Novickij V, Malyško V, Želvys A, Balevičiūtė A, Zinkevičienė A, Novickij J, et al. Electrochemotherapy using doxorubicin and nanosecond electric field pulses: a pilot in vivo study. Molecules 2020; 25: 4601.
|
| [7] |
Qi Y, Sun D, Wang L, Yu J, Liang P. State-of-the-art and development trend of interventional ultrasound in China. Advanced Ultrasound in Diagnosis and Therapy 2023; 7: 313-320.
|
| [8] |
Batista Napotnik T, Polajžer T, Miklavčič D. Cell death due to electroporation - a review. Bioelectrochemistry 2021; 141: 107871.
|
| [9] |
Michel O, Pakhomov AG, Casciola M, Saczko J, Kulbacka J, Pakhomova ON. Electropermeabilization does not correlate with plasma membrane lipid oxidation. Bioelectrochemistry 2020; 132: 107433.
|
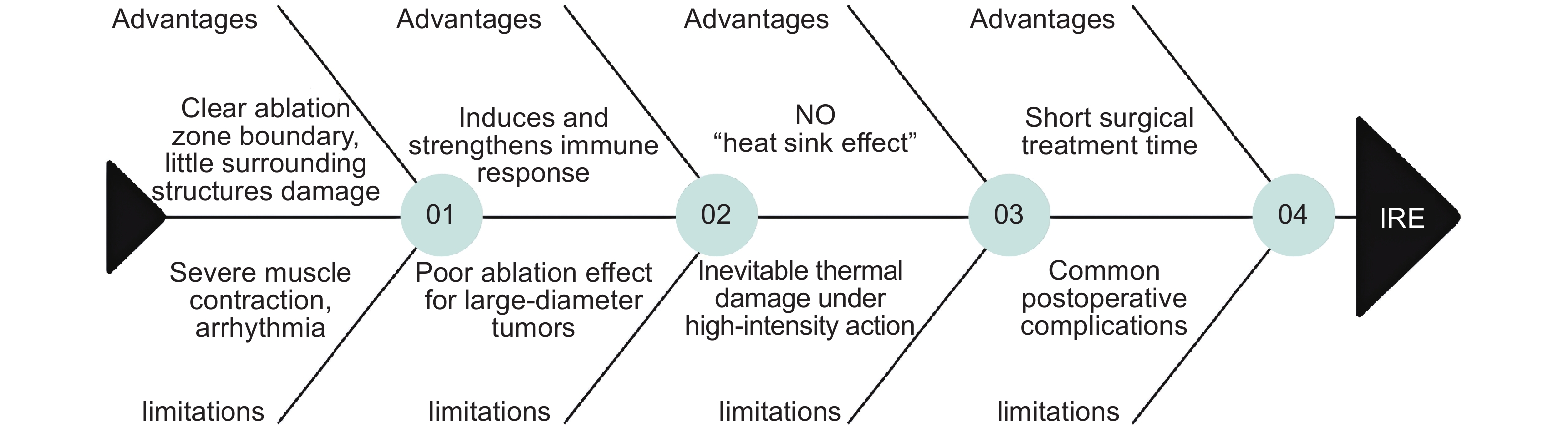
| [10] |
Maccarrone M, Bladergroen MR, Rosato N, Finazzi Agrò AF. Role of lipid peroxidation in electroporation-induced cell permeability. Biochem Bioph Res Co 1995; 209: 417-425.
|
| [11] |
Kotnik T, Miklavcic D. Theoretical evaluation of voltage inducement on internal membranes of biological cells exposed to electric fields. Biophys J 2006; 90: 480-491.
|
| [12] |
Kotnik T, Rems L, Tarek M, Miklavčič D. Membrane electroporation and electropermeabilization: mechanisms and models. Annu rev biophys 2019; 48: 63-91.
|
| [13] |
Ringel-Scaia VM, Beitel-White N, Lorenzo MF, Brock RM, Huie KE, Coutermarsh-Ott S, et al. High-frequency irreversible electroporation is an effective tumor ablation strategy that induces immunologic cell death and promotes systemic anti-tumor immunity. EBioMedicine 2019; 44: 112-125.
|
| [14] |
Mi Y, Sun C, Yao C, Xiong L, Wang S, Luo X, et al. [Effect of steep pulsed electric fields on the immune response of tumor-bearing Wistar mice]. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 2007; 24: 253-256.
|
| [15] |
Mi Y, Sun C, Yao C, Xiong L, Wang S, Li C, et al. Lethal effects of Steep Pulsed Electric Field (SPEF) to Target Lymphatic Capillaries in VX2Implanted Breast Cancer of Rabbits. Conf Proc IEEE Eng Med Biol Soc 2005; 2005: 4904-4907.
|
| [16] |
Bulvik BE, Rozenblum N, Gourevich S, Ahmed M, Andriyanov AV, Galun E, et al. , Irreversible electroporation versus radiofrequency ablation: a comparison of local and systemic effects in a small-animal model. Radiology 2016; 280: 413-424.
|
| [17] |
Imran KM, Nagai-Singer MA, Brock RM, Alinezhadbalalami N, Davalos RV, Allen IC. Exploration of novel pathways underlying irreversible electroporation induced anti-tumor immunity in pancreatic cancer. Front Oncol 2022; 12: 853779.
|
| [18] |
Zhang N, Li Z, Han X, Zhu Z, Li Z, Zhao Y, et al. Irreversible electroporation: an emerging immunomodulatory therapy on solid tumors. Front Immunol 2021; 12: 811726.
|
| [19] |
Yao C, Lv Y, Dong S, Zhao Y, Liu H. Irreversible electroporation ablation area enhanced by synergistic high- and low-voltage pulses. PLoS One 2017; 12: e0173181.
|
| [20] |
Weaver JC, Smith KC, Esser AT, Son RS, Gowrishankar TR. A brief overview of electroporation pulse strength-duration space: a region where additional intracellular effects are expected. Bioelectrochemistry 2012; 87: 236-243.
|
| [21] |
Jiang C, Qin Z, Bischof J. Membrane-targeting approaches for enhanced cancer cell destruction with irreversible electroporation. Ann Biomed Eng 2014; 42: 193-204.
|
| [22] |
Li C, Yao C, Sun C, Guo F, Zhou W, Xiong Z. Dependence on electric field intensities of cell biological effects induced by microsecond pulsed electric fields. IEEE Trans Dielectr Electr Insul 2011; 18: 2083-2088.
|
| [23] |
Sano MB, Neal RE 2nd, Garcia PA, Gerber D, Robertson J, Davalos RV. Towards the creation of decellularized organ constructs using irreversible electroporation and active mechanical perfusion. Biomed Eng Online 2010; 9: 83.
|
| [24] |
Mi Y, Xu J, Liu Q, Wu X, Zhang Q, Tang J. Single-cell electroporation with high-frequency nanosecond pulse bursts: simulation considering the irreversible electroporation effect and experimental validation. Bioelectrochemistry 2021; 140: 107822.
|
| [25] |
Peng W, Cao Y, Zhang Y, Zhong A, Zhang C, Wei Z, et al. Optimal irreversible electroporation combined with nano-enabled immunomodulatory to boost systemic antitumor immunity. Adv Healthc Mater 2024; 13: e2302549.
|
| [26] |
Sano MB, Fesmire CC, DeWitt MR, Xing L. Burst and continuous high frequency irreversible electroporation protocols evaluated in a 3D tumor model. Phys Med Biol 2018; 63: 135022.
|
| [27] |
Davalos RV, Mir IL, Rubinsky B. Tissue ablation with irreversible electroporation. Ann Biomed Eng 2005; 33: 223-231.
|
| [28] |
Al-Sakere B, André F, Bernat C, Connault E, Opolon P, Davalos RV, et al. Tumor ablation with irreversible electroporation. PLoS One 2007; 2: e1135.
|
| [29] |
Guo Y, Zhang Y, Klein R, Nijm GM, Sahakian AV, Omary RA, et al. Irreversible electroporation therapy in the liver: longitudinal efficacy studies in a rat model of hepatocellular carcinoma. Cancer Res 2010; 70: 1555-1563.
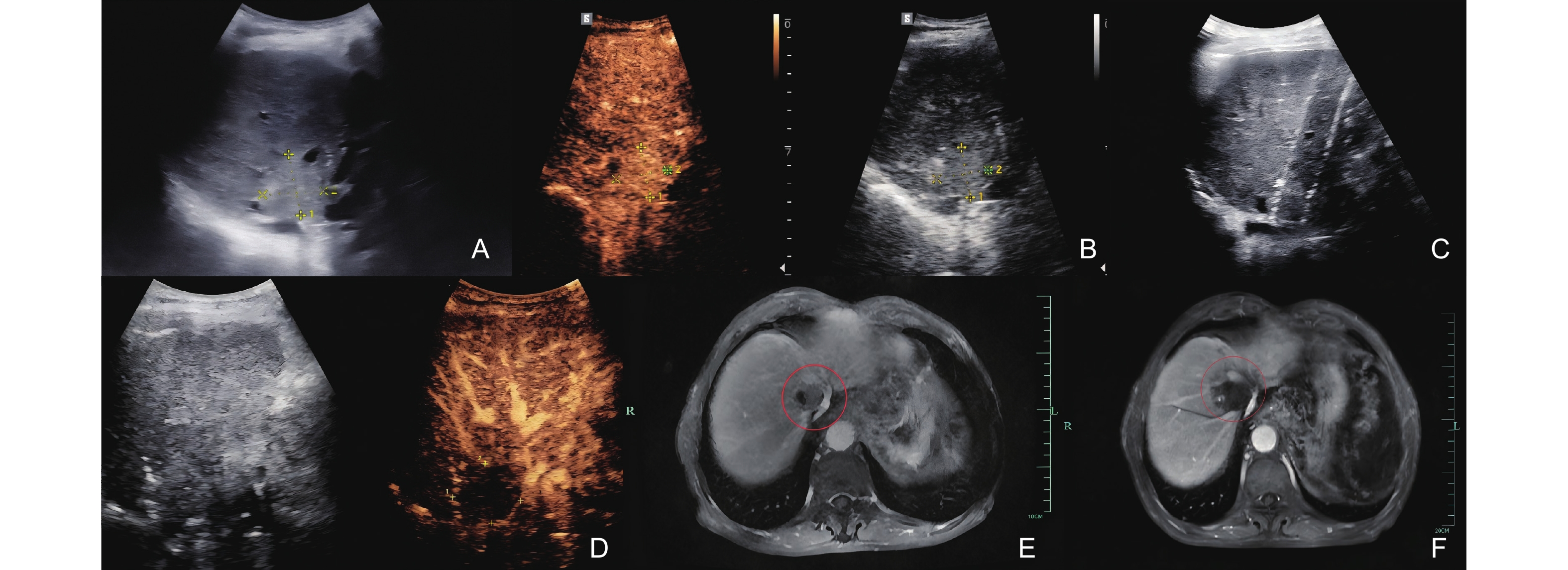
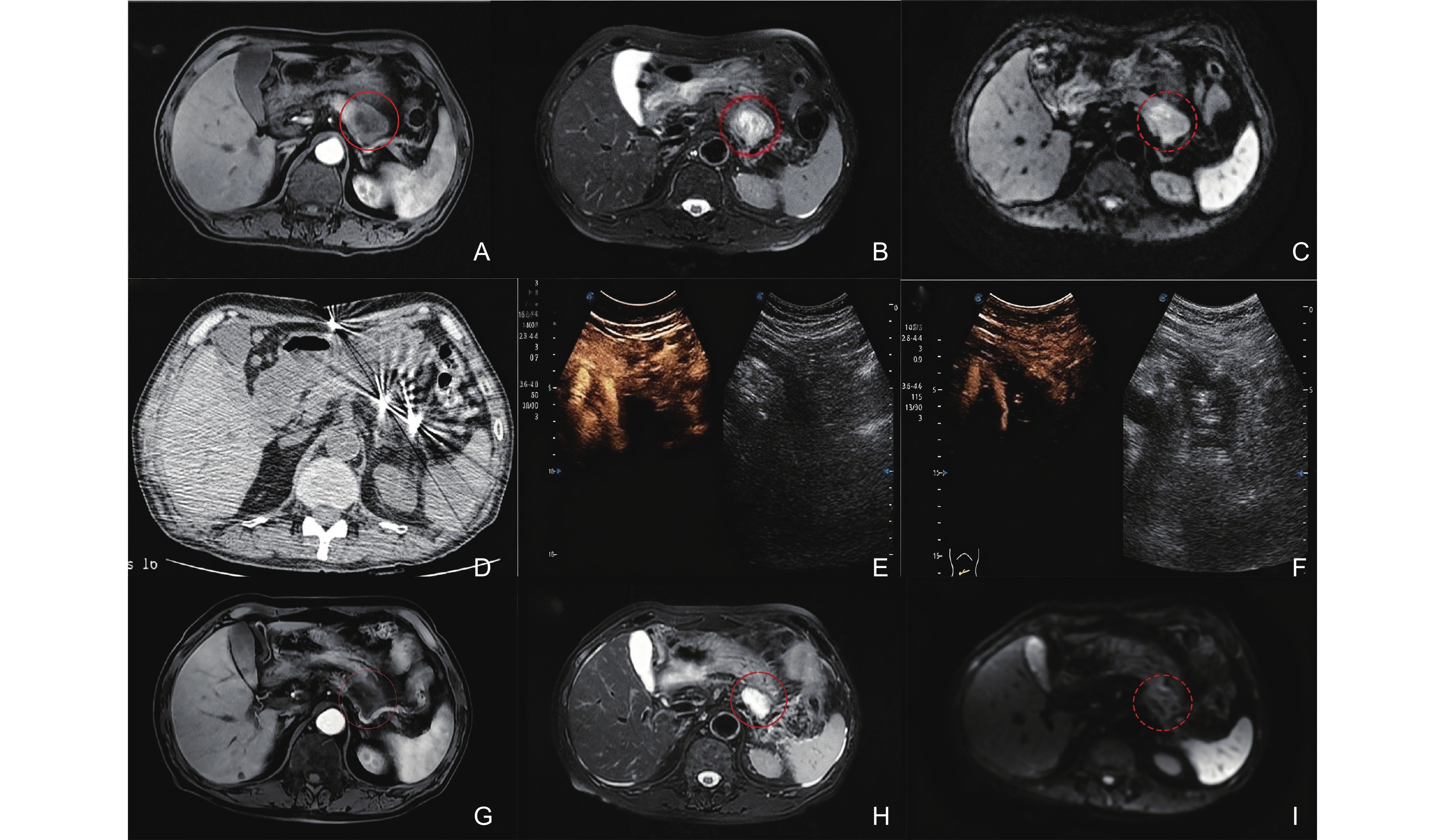
|
| [30] |
Lee EW, Chen C, Prieto VE, Dry SM, Loh CT, Kee ST. Advanced hepatic ablation technique for creating complete cell death: irreversible electroporation. Radiology 2010; 255: 426-433.
|
| [31] |
Bower M, Sherwood L, Li Y, Martin R. Irreversible electroporation of the pancreas: definitive local therapy without systemic effects. J Surg Oncol 2011; 104: 22-28.
|
| [32] |
Onik G, Mikus P, Rubinsky B. Irreversible electroporation: implications for prostate ablation. Technol Cancer Res Treat 2007; 6: 295-300.
|
| [33] |
Maor E, Ivorra A, Leor J, Rubinsky B. The effect of irreversible electroporation on blood vessels. Technol Cancer Res Treat 2007; 6: 307-312.
|
| [34] |
Kim HB, Sung CK, Baik KY, Moon KW, Kim HS, Yi JH, et al. Changes of apoptosis in tumor tissues with time after irreversible electroporation. Biochem Biophys Res Commun 2013; 435: 651-656.
|
| [35] |
Liu Y, Xiong Z, Zhou W, Hua Y, Li C, Yao C. Percutaneous ultrasound-guided irreversible electroporation: a goat liver study. Oncol Lett 2012; 4: 450-454.
|
| [36] |
Jeon SM, Davaa E, Jiang Y, Jenjob R, Truong NT, Shin KJ, et al. Assessment of hepatic lesions after non-thermal tumor ablation by irreversible electroporation in a pig model. Technol Cancer Res Treat 2023; 22: 15330338221147122.
|
| [37] |
Sorokin I, Canvasser N, Johnson B, Lucas E, Cadeddu JA. Irreversible electroporation for renal ablation does not cause significant injury to adjacent ureter or bowel in a porcine model. J Endourol 2021; 35: 873-877.
|
| [38] |
Olweny EO, Kapur P, Tan YK, Park SK, Adibi M, Cadeddu JA. Irreversible electroporation: evaluation of nonthermal and thermal ablative capabilities in the porcine kidney. Urology 2013; 81: 679-684.
|
| [39] |
Yan L, Liang B, Feng J, Zhang HY, Chang HS, Liu B, et al. Safety and feasibility of irreversible electroporation for the pancreatic head in a porcine model. World J Gastrointest Oncol 2022; 14: 1499-1509.
|
| [40] |
Lee EW, Shahrouki P, Peterson S, Tafti BA, Ding PX, Kee ST. Safety of irreversible electroporation ablation of the pancreas. Pancreas 2021; 50: 1281-1286.
|
| [41] |
Zhao J, Wen X, Tian L, Li T, Xu C, Wen X, et al. Irreversible electroporation reverses resistance to immune checkpoint blockade in pancreatic cancer. Nat Commun 2019; 10: 899.
|
| [42] |
Blazevski A, Scheltema MJ, Amin A, Thompson JE, Lawrentschuk N, Stricker PD. Irreversible electroporation (IRE): a narrative review of the development of IRE from the laboratory to a prostate cancer treatment. Bju Int 2020; 125: 369-378.
|
| [43] |
Phillips MA, Narayan R, Padath T, Rubinsky B. Irreversible electroporation on the small intestine. Brit J Cancer 2012; 106: 490-495.
|
| [44] |
Garcia PA, Rossmeisl JH Jr, Robertson J, Ellis TL, Davalos RV. Pilot study of irreversible electroporation for intracranial surgery. Annu Int Conf IEEE Eng Med Biol Soc 2009; 2009: 6513-6516.
|
| [45] |
Thomson K. Human experience with irreversible electroporation, in irreversible electroporation. Springer Berlin Heidelberg: Berlin, Heidelberg 2010; 249-254.
|
| [46] |
Thomson K, Kee ST. Clinical research on irreversible electroporation of the liver, in clinical aspects of electroporation. Springer New York: New York, NY 2011; 237-246.
|
| [47] |
Philips P, Hays D, Martin RC. Irreversible electroporation ablation (IRE) of unresectable soft tissue tumors: learning curve evaluation in the first 150 patients treated. PLoS One 2013; 8: e76260.
|
| [48] |
Niessen C, Beyer LP, Pregler B, Dollinger M, Trabold B, Schlitt HJ, et al. Percutaneous ablation of hepatic tumors using irreversible electroporation: a prospective safety and midterm efficacy study in 34 patients. J Vasc Interv Radiol 2016; 27: 480-486.
|
| [49] |
Distelmaier M, Barabasch A, Heil P, Kraemer NA, Isfort P, Keil S, et al. Midterm safety and efficacy of irreversible electroporation of malignant liver tumors located close to major portal or hepatic veins. Radiology 2017; 285: 1023-1031.
|
| [50] |
Frühling P, Stillström D, Holmquist F, Nilsson A, Freedman J. Irreversible electroporation of hepatocellular carcinoma and colorectal cancer liver metastases: a nationwide multicenter study with short- and long-term follow-up. Eur J Surg Oncol 2023; 49: 107046.
|
| [51] |
Bhutiani N, Philips P, Scoggins CR, McMasters KM, Potts MH, Martin RC. Evaluation of tolerability and efficacy of irreversible electroporation (IRE) in treatment of Child-Pugh B (7/8) hepatocellular carcinoma (HCC). Hpb 2016; 18: 593-599.
|
| [52] |
Hassany M, Mahboub AM, Mostafa W, Debian H, Shousha HI, El-Serafy M. Assessment of efficacy and safety of irreversible electroporation versus TACE for treatment of difficult location hepatocellular carcinoma. Egypt Liver J 2024; 14: 1-11.
|
| [53] |
Alnaggar M, Lin M, Mesmar A, Liang S, Qaid A, Xu K, et al. Allogenic natural killer cell immunotherapy combined with irreversible electroporation for stage IV hepatocellular carcinoma: survival outcome. Cell Physiol Biochem 2018; 48: 1882-1893.
|
| [54] |
Yang Y, Qin Z, Du D, Wu Y, Qiu S, Mu F, et al. Safety and short-term efficacy of irreversible electroporation and allogenic natural killer cell immunotherapy combination in the treatment of patients with unresectable primary liver cancer. Cardiovasc Inter Rad 2019; 42: 48-59.
|
| [55] |
Meijerink M. R., etal. Irreversible Electroporation to Treat Unresectable Colorectal Liver Metastases (COLDFIRE-2): A Phase II, Two-Center, Single-Arm Clinical Trial. Radiology, 2021; 299 2 470-480.
|
| [56] |
Meijerink MR, Ruarus AH, Vroomen LGPH, Puijk RS, Geboers B, Nieuwenhuizen S, et al. Peri-tumoral metallic implants reduce the efficacy of irreversible electroporation for the ablation of colorectal liver metastases. Cardiovasc Inter Rad 2020; 43: 84-93.
|
| [57] |
Niessen C, Thumann S, Beyer L, Pregler B, Kramer J, Lang S, et al. Percutaneous irreversible electroporation: long-term survival analysis of 71 patients with inoperable malignant hepatic tumors. Sci Rep 2017; 7: 43687.
|
| [58] |
Frühling P, Nilsson A, Duraj F, Haglund U, Norén A. Single-center nonrandomized clinical trial to assess the safety and efficacy of irreversible electroporation (IRE) ablation of liver tumors in humans: short to mid-term results. Ejso-eur J Surg Onc 2017; 43: 751-757.
|
| [59] |
Hosein PJ, Echenique A, Loaiza-Bonilla A, Froud T, Barbery K, Rocha Lima CM, et al. Percutaneous irreversible electroporation for the treatment of colorectal cancer liver metastases with a proposal for a new response evaluation system. J Vasc Interv Radiol 2014; 25: 1233-1239.
|
| [60] |
Ruarus AH, Vroomen LGPH, Geboers B, van Veldhuisen E, Puijk RS, Nieuwenhuizen S, et al. Percutaneous irreversible electroporation in locally advanced and recurrent pancreatic cancer (PANFIRE-2): a multicenter, prospective, single-arm, phase II study. Radiology 2020; 294: 212-220.
|
| [61] |
Li SP, He CB, Wang J, Mao YZ, Lao XM, Cui BK, et al. [Combining intraoperative ultrasound-guided irreversible electroporation with chemotherapy for treating locally advanced pancreatic cancer: a clinical report of 64 cases]. Zhonghua Wai Ke Za Zhi 2020; 58: 787-792.
|
| [62] |
Yan L, Chen YL, Su M, Liu T, Xu K, Liang F, et al. A single-institution experience with open irreversible electroporation for locally advanced pancreatic carcinoma. Chinese Med J-Peking 2016; 129: 2920-2925.
|
| [63] |
Scheffer HJ, Vroomen LG, de Jong MC, Melenhorst MC, Zonderhuis BM, Daams F, et al. Ablation of locally advanced pancreatic cancer with percutaneous irreversible electroporation: results of the phase I/II PANFIRE study. Radiology 2017; 282: 585-597.
|
| [64] |
Martin RC 2nd, McFarland K, Ellis S, Velanovich V. Irreversible electroporation in locally advanced pancreatic cancer: potential improved overall survival. Ann Surg Oncol 2013; 20 suppl 3: S443-449.
|
| [65] |
Narayanan G, Hosein PJ, Beulaygue IC, Froud T, Scheffer HJ, Venkat SR, et al. Percutaneous image-guided irreversible electroporation for the treatment of unresectable, locally advanced pancreatic adenocarcinoma. J Vasc Interv Radiol 2017; 28: 342-348.
|
| [66] |
Narayanan G, Bilimoria MM, Hosein PJ, Su Z, Mortimer KM, Martin RCG 2nd. Multicenter randomized controlled trial and registry study to assess the safety and efficacy of the NanoKnife® system for the ablation of stage 3 pancreatic adenocarcinoma: overview of study protocols. BMC Cancer 2021; 21: 785.
|
| [67] |
Lin M, Liang S, Wang X, Liang Y, Zhang M, Chen J, et al. Percutaneous irreversible electroporation combined with allogeneic natural killer cell immunotherapy for patients with unresectable (stage III/IV) pancreatic cancer: a promising treatment. J Cancer Res Clin 2017; 143: 2607-2618.
|
| [68] |
Lin M, Zhang X, Liang S, Luo H, Alnaggar M, Liu A, et al. Irreversible electroporation plus allogenic Vγ9Vδ2 T cells enhances antitumor effect for locally advanced pancreatic cancer patients. Signal Transduct Tar 2020; 5: 215.
|
| [69] |
O'Neill C, Hayat T, Hamm J, Healey M, Zheng Q, Li Y, et al. A phase 1b trial of concurrent immunotherapy and irreversible electroporation in the treatment of locally advanced pancreatic adenocarcinoma. Surgery 2020; 168: 610-616.
|
| [70] |
Pan Q, Hu C, Fan Y, Wang Y, Li R, Hu X. Efficacy of irreversible electroporation ablation combined with natural killer cells in treating locally advanced pancreatic cancer. J Buon 2020; 25: 1643-1649.
|
| [71] |
Ma Y, Xing Y, Li H, Yuan T, Liang B, Li R, et al. Irreversible electroporation combined with chemotherapy and PD-1/PD-L1 blockade enhanced antitumor immunity for locally advanced pancreatic cancer. Front Immunol 2023; 14: 1193040.
|
| [72] |
Onik G, Rubinsky B. Irreversible electroporation: first patient experience focal therapy of prostate cancer, in irreversible electroporation. Springer Berlin Heidelberg: Berlin, Heidelberg 2010; 235-247.
|
| [73] |
Ting F, Tran M, Böhm M, Siriwardana A, Van Leeuwen PJ, Haynes AM, et al. Focal irreversible electroporation for prostate cancer: functional outcomes and short-term oncological control. Prostate Cancer Prostatic Dis 2016; 19: 46-52.
|
| [74] |
Wang H, Xue W, Yan W, Yin L, Dong B, He B, et al. Extended focal ablation of localized prostate cancer with high-frequency irreversible electroporation: a nonrandomized controlled trial. JAMA Surg 2022; 157: 693-700.
|
| [75] |
Scheltema MJ, Geboers B, Blazevski A, Doan P, Katelaris A, Agrawal S, et al. Median 5-year outcomes of primary focal irreversible electroporation for localised prostate cancer. Bju Int 2023; 131 suppl 4: 6-13.
|
| [76] |
Dong S, Wang H, Zhao Y, Sun Y, Yao C. First human trial of high-frequency irreversible electroporation therapy for prostate cancer. Technol Cancer Res Treat 2018; 17: 1533033818789692.
|
| [77] |
Fenner A. Prostate cancer: irreversible electroporation is a safe and feasible option for focal therapy. Nat Rev Urol 2014; 11: 600.
|
| [78] |
Wah TM, Lenton J, Smith J, Bassett P, Jagdev S, Ralph C, et al. Irreversible electroporation (IRE) in renal cell carcinoma (RCC): a mid-term clinical experience. Eur Radiol 2021; 31: 7491-7499.
|
| [79] |
Wang Z, Lu J, Huang W, Wu Z, Gong J, Wang Q, et al. A retrospective study of CT-guided percutaneous irreversible electroporation (IRE) ablation: clinical efficacy and safety. BMC Cancer 2021; 21: 124.
|
| [80] |
Buijs M, Zondervan PJ, de Bruin DM, van Lienden KP, Bex A, van Delden OM. Feasibility and safety of irreversible electroporation (IRE) in patients with small renal masses: results of a prospective study. Urol Oncol 2019; 37: 183.e1-183.e8.
|
| [81] |
Ben-David E, Ahmed M, Faroja M, Moussa M, Wandel A, Sosna J, et al. Irreversible electroporation: treatment effect is susceptible to local environment and tissue properties. Radiology 2013; 269: 738-747.
|
| [82] |
Rai ZL, Feakins R, Pallett LJ, Manas D, Davidson BR. Irreversible electroporation (IRE) in locally advanced pancreatic cancer: a review of current clinical outcomes, mechanism of action and opportunities for synergistic therapy. J Clin Med 2021; 10: 1609.
|
| [83] |
Srimathveeravalli G, Wimmer T, Silk M, Sofocleous CT, Erinjeri JP, Solomon SB. Treatment planning considerations for IRE in the lung: placement of needle electrodes is critical. J Vasc Interv Radiol 2013; 24: S22.
|
| [84] |
Fuhrmann I, Probst U, Wiggermann P, Beyer L. Navigation systems for treatment planning and execution of percutaneous irreversible electroporation. Technol Cancer Res Treat 2018; 17: 1533033818791792.
|
| [85] |
Westwood M, Joore M, Grutters J, Redekop K, Armstrong N, Lee K, et al. Contrast-enhanced ultrasound using SonoVue® (sulphur hexafluoride microbubbles) compared with contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging for the characterisation of focal liver lesions and detection of liver metastases: a systematic review and cost-effectiveness analysis. Health Technol Asses 2013; 17: 1-243.
|
| [86] |
Appelbaum L, Ben-David E, Sosna J, Nissenbaum Y, Goldberg SN. US findings after irreversible electroporation ablation: radiologic-pathologic correlation. Radiology 2012; 262: 117-125.
|
| [87] |
Schmidt CR, Shires P, Mootoo M. Real-time ultrasound imaging of irreversible electroporation in a porcine liver model adequately characterizes the zone of cellular necrosis. Hpb 2012; 14: 98-102.
|
| [88] |
Lu MD, Yu XL, Li AH, Jiang TA, Chen MH, Zhao BZ, et al. Comparison of contrast enhanced ultrasound and contrast enhanced CT or MRI in monitoring percutaneous thermal ablation procedure in patients with hepatocellular carcinoma: a multi-center study in China. Ultrasound Med Biol 2007; 33: 1736-1749.
|
| [89] |
Zhang GY, Tang Y, Wang MY, Kong WN. Diagnostic utility of superb microvascular imaging of ultrasound examinations to evaluate hepatic ischemia-reperfusion injury. Advanced Ultrasound in Diagnosis and Therapy 2024; 8: 15-21.
|
| [90] |
Mahmoud O, Makkena A, Wessner CE, Liu JB, Eisenbrey JR, Lyshchik A. Contrast-Enhanced Ultrasound LI-RADS: a pictorial review. Advanced Ultrasound in Diagnosis and Therapy 2023; 7: 321-332.
|
| [91] |
Ball C, Thomson KR, Kavnoudias H. Irreversible electroporation: a new challenge in "out of operating theater" anesthesia. Anesth Analg 2010; 110: 1305-1309.
|
| [92] |
Cheung W, Kavnoudias H, Roberts S, Szkandera B, Kemp W, et al. Irreversible electroporation for unresectable hepatocellular carcinoma: initial experience and review of safety and outcomes. Technol Cancer Res Treat 2013; 12: 233-241.
|
| [93] |
Guo Y, Zhang Y, Nijm GM, Sahakian AV, Yang GY, Omary RA, et al. Irreversible electroporation in the liver: contrast-enhanced inversion-recovery MR imaging approaches to differentiate reversibly electroporated penumbra from irreversibly electroporated ablation zones. Radiology 2011; 258: 461-468.
|
| [94] |
Wendler JJ, Pech M, Porsch M, Janitzky A, Fischbach F, Buhtz P, et al. Urinary tract effects after multifocal nonthermal irreversible electroporation of the kidney: acute and chronic monitoring by magnetic resonance imaging, intravenous urography and urinary cytology. Cardiovasc Inter Rad 2012; 35: 921-926.
|
| [95] |
Wagstaff PG, Buijs M, van den Bos W, de Bruin DM, Zondervan PJ, de la Rosette JJ, et al. Irreversible electroporation: state of the art. Onco Targets Ther 2016; 9: 2437-2446.
|
| [96] |
Al-Sakere B, Bernat C, Andre F, Connault E, Opolon P, Davalos RV, et al. A study of the immunological response to tumor ablation with irreversible electroporation. Technol Cancer Res Treat 2007; 6: 301-306.
|
| [97] |
Narayanan JSS, Ray P, Hayashi T, Whisenant TC, Vicente D, Carson DA, et al. Irreversible electroporation combined with checkpoint blockade and TLR7 stimulation induces antitumor immunity in a murine pancreatic cancer model. Cancer Immunol Res 2019; 7: 1714-1726.
|
| [98] |
Burbach BJ, O'Flanagan SD, Shao Q, Young KM, Slaughter JR, Rollins MR, et al. Irreversible electroporation augments checkpoint immunotherapy in prostate cancer and promotes tumor antigen-specific tissue-resident memory CD8+ T cells. Nat Commun 2021; 12: 3862.
|
| [99] |
Neal RE, Davalos RV. The feasibility of irreversible electroporation for the treatment of breast cancer and other heterogeneous systems. Ann Biomed Eng 2009; 37: 2615-2625.
|
| [100] |
Niessen C, Igl J, Pregler B, Beyer L, Noeva E, Dollinger M, et al. , Factors associated with short-term local recurrence of liver cancer after percutaneous ablation using irreversible electroporation: a prospective single-center study. J Vasc Interv Radiol 2015; 26: 694-702.
|
| [101] |
Spiliopoulos S, Reppas L, Filippiadis D, Delvecchio A, Conticchio M, Memeo R, et al. Irreversible electroporation for the management of pancreatic cancer: Current data and future directions. World J Gastroentero 2023; 29: 223-231.
|
| [102] |
Faroja M, Ahmed M, Appelbaum L, Ben-David E, Moussa M, Sosna J, et al. Irreversible electroporation ablation: is all the damage nonthermal? Radiology 2013; 266: 462-470.
|
| [103] |
Timmer FEF, Geboers B, Ruarus AH, Schouten EAC, Nieuwenhuizen S, Puijk RS, et al. Irreversible electroporation for locally advanced pancreatic cancer. Tech Vasc Interv Rad 2020; 23: 100675.
|
| [104] |
Tasu JP, Tougeron D, Rols MP. Irreversible electroporation and electrochemotherapy in oncology: state of the art. Diagn Interv Imaging 2022; 103: 499-509.
|
| [105] |
Martin RC 2nd, Kwon D, Chalikonda S, Sellers M, Kotz E, Scoggins C, et al. Treatment of 200 locally advanced (stage III) pancreatic adenocarcinoma patients with irreversible electroporation: safety and efficacy. Ann Surg 2015; 262: 486-494.
|
| [106] |
Martin RC 2nd, Kwon D, Chalikonda S, Sellers M, Kotz E, Scoggins C, et al. Early nontumorous CT findings after irreversible electroporation of locally advanced pancreatic cancer. Abdom Radiol 2016; 41: 2142-2149.
|
| [107] |
Tian G, Liu X, Zhao Q, Xu D, Jiang T. Irreversible electroporation in patients with pancreatic cancer: how important is the new weapon? Biomed Res Int 2018; 2018: 5193067.
|
| [108] |
Forde PF, Sadadcharam M, Bourke MG, Conway TA, Guerin SR, de Kruijf M, et al. Preclinical evaluation of an endoscopic electroporation system. Endoscopy 2016; 48: 477-483.
|
| [109] |
Ueshima E, Schattner M, Mendelsohn R, Gerdes H, Monette S, Takaki H, et al. Transmural ablation of the normal porcine common bile duct with catheter-directed irreversible electroporation is feasible and does not affect duct patency. Gastrointest Endosc 2018; 87: 300.e1-300.e6.
|
| [110] |
Kodama H, Vroomen LG, Ueshima E, Reilly J, Brandt W, Paluch LR, et al. Catheter-based endobronchial electroporation is feasible for the focal treatment of peribronchial tumors. J Thorac Cardiov Sur 2018; 155: 2150-2159.
|
| [111] |
Ren F, Li Q, Hu L, Yan X, Gao Z, Zhang J, et al. Safety and efficacy of magnetic anchoring electrode-assisted irreversible electroporation for gastric tissue ablation. Surg Endosc 2020; 34: 580-589.
|
| [112] |
Arena CB, Szot CS, Garcia PA, Rylander MN, Davalos RV. A three-dimensional in vitro tumor platform for modeling therapeutic irreversible electroporation. Biophys J 2012; 103: 2033-2042.
|
| [113] |
Edd JF, Davalos RV. Mathematical modeling of irreversible electroporation for treatment planning. Technol Cancer Res Treat 2007; 6: 275-286.
|
| [114] |
Pavliha D, Kos B, Marčan M, Zupanič A, Serša G, Miklavčič D. Planning of electroporation-based treatments using web-based treatment-planning software. J Membrane Biol 2013; 246: 833-842.
|
| [115] |
Kos B, Voigt P, Miklavcic D, Moche M. Careful treatment planning enables safe ablation of liver tumors adjacent to major blood vessels by percutaneous irreversible electroporation (IRE). Radiol Oncol 2015; 49: 234-241.
|