Advanced Ultrasound in Diagnosis and Therapy ›› 2025, Vol. 9 ›› Issue (4): 375-387.doi: 10.26599/AUDT.2025.250094
Previous Articles Next Articles
Guan Xina,1, Hu Xinyuanb,1, Han Hongb, Zhang Dezhic,*( ), Xu Huixionga,*(
), Xu Huixionga,*( )
)
Received:2025-09-12
Revised:2025-09-24
Accepted:2025-10-20
Online:2025-12-30
Published:2025-11-06
Contact:
Abdominal Ultrasound Department, Diagnostic Ultrasound Center, First Hospital of Jilin University, Jilin, P. R. China (Dezhi Zhang), e-mail: dezhi@jlu.edu.cn (DZ Z);Department of Ultrasound, Zhongshan Hospital (Xiamen), Fudan University, Xiamen, 361000, China (Huixiong Xu),e-mail: xuhuixiong@126.com (HX X).,
About author:1Xin Guan and Xinyuan Hu contributed equally to this study.
Guan Xin, Hu Xinyuan, Han Hong, Zhang Dezhi, Xu Huixiong. The Evolving Application of Ultrasound in the Precision Management of Small Hepatocellular Carcinoma. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 375-387.

Figure 1
Emerging ultrasound techniques and algorithms for the management of small HCC. US, ultrasound; CEUS, contrast-enhanced ultrasound; LI-RADS, liver imaging reporting and data system; TRA, treatment response assessment; HCC, hepatocellular carcinoma. Reproduced with permission from [57,60] and [67]."
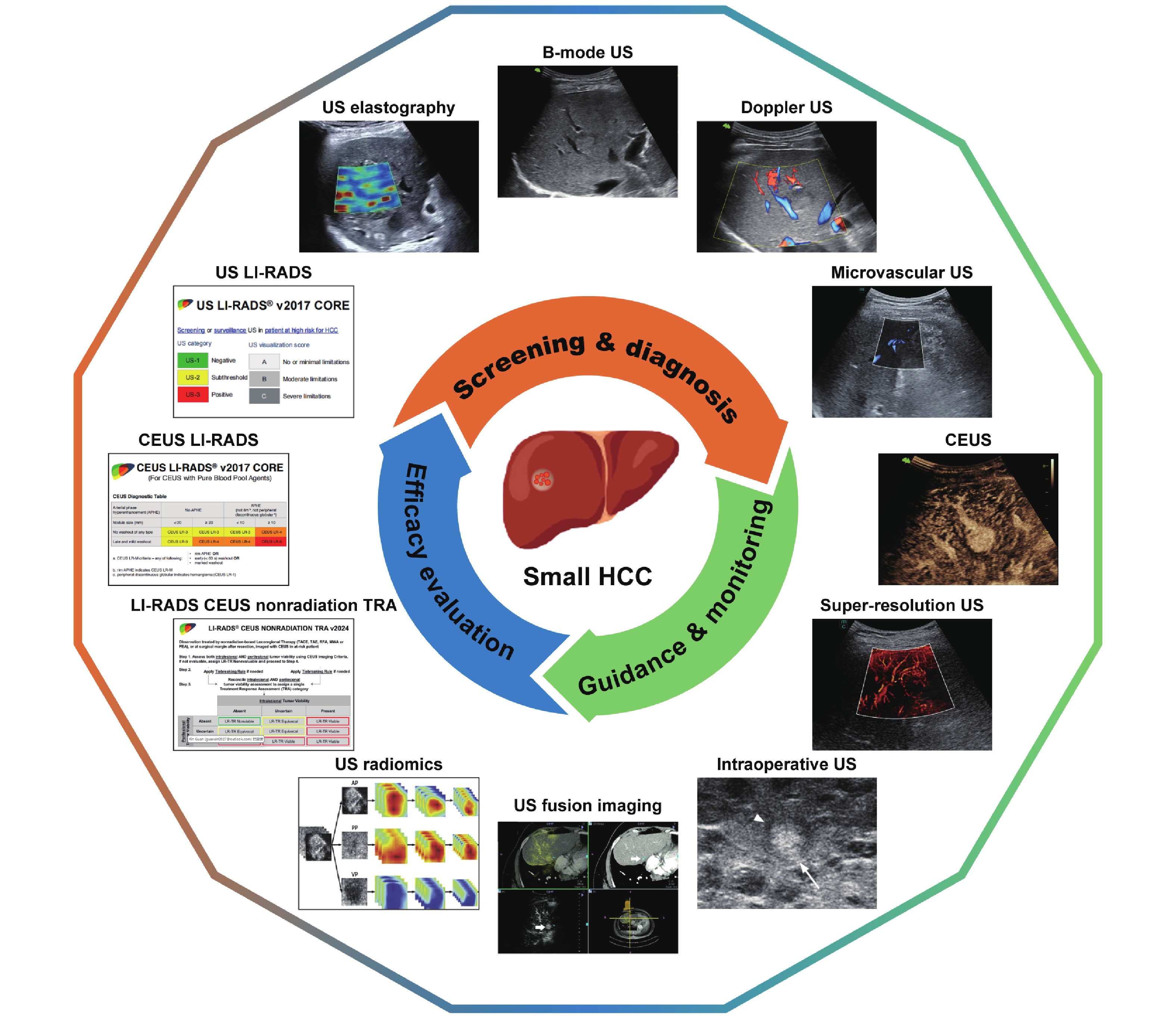
Table 1
Comparison of major clinical guidelines for the diagnosis of small HCC"
| Guidelines | EASL | AASLD | APASL | CSH | KLCA | JSH |
| EASL, the European Association for the Study of the Liver; AASLD, the American Association for the Study of Liver Diseases; APASL, the Asia-Pacific Association for the Study of the Liver; CSH, the Chinese Society for the Study of the Liver; KLCA-NCC, the Korean Liver Cancer Association-National Cancer Center; JSH, the Japanese Society for the Study of the Liver; CT, computed tomography; MRI, magnetic resonance imaging; CEUS, con trast-enhanced ultrasound; HBA, hepatobiliary agents; LI-RADS, Liver Imaging Reporting and Data System. | ||||||
| Imaging modality | CT/MRI | CT/MRI | CT/MRI/CEUS | CT/MRI/CEUS | CT/MRI/CEUS | CT/MRI/CEUS |
| CEUS role | Secondary | Secondary | First-line | First-line | First-line | First-line |
| HBA-MRI role | Recognized, optional | Recognized, optional | Recognized, optional | Recommended, widely used | Integral to algorithm | Integral to algorithm |
| Diagnostic algorithm | EASL Criteria | LI-RADS | APASL Criteria | China Criteria | KLCA Criteria | JSH Criteria |
| Diagnosis for ≤ 2 cm nodule | Typical pattern on 1 technique | Typical pattern on 1 technique | Typical pattern on 1 technique | Typical pattern on 1 technique | Typical pattern on 1 technique | Often typical pattern on 1 technique |
| Biopsy for atypical ≤ 2 cm nodule | Recommended | Recommended | Consider alternative imaging first | Consider alternative imaging first | Consider alternative imaging first | Consider alternative imaging first |

Figure 2
Major pathologic changes of liver nodules during hepatocarcinogenesis and associated ultrasonographic manifestations. RN, regenerative nodule; LGDN, low-grade dysplastic nodule; HGDN, high-grade dysplastic nodule; HCC, hepatocellular carcinoma; US, ultrasound; APHE, arterial phase hyper enhancement; KP, Kupffer phase."
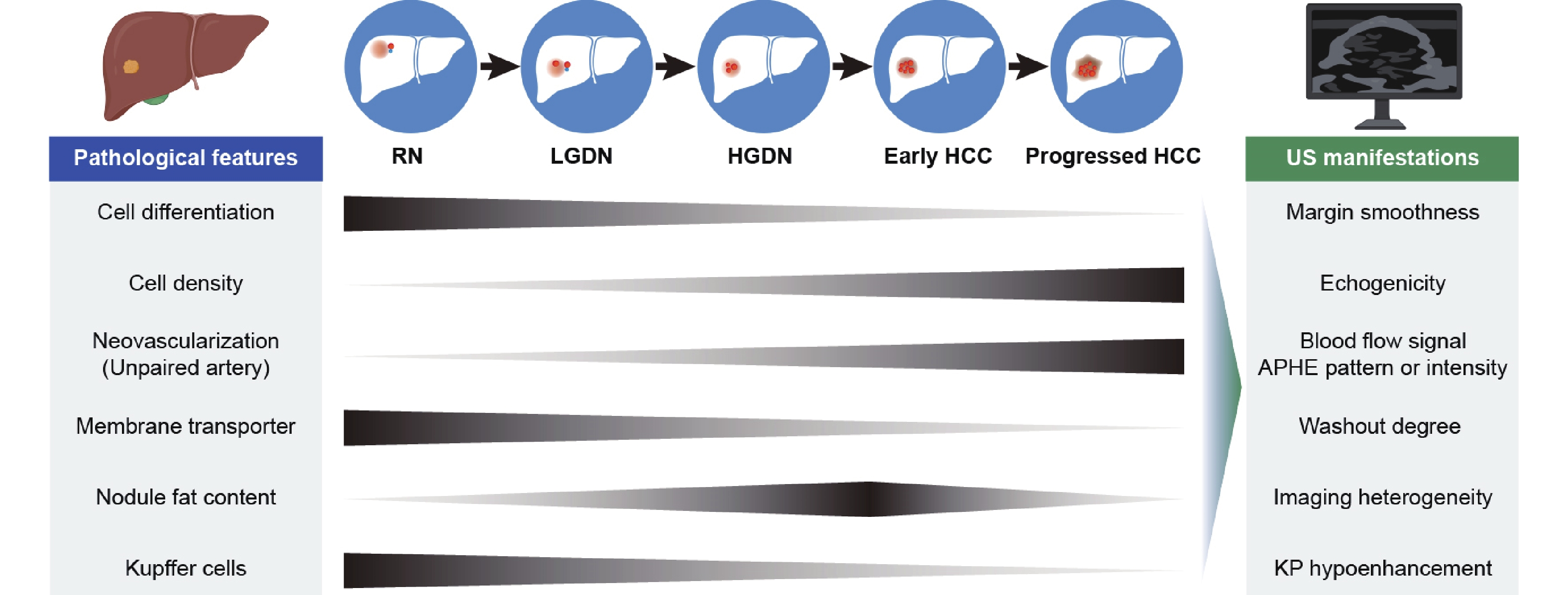
Table 2
Comparison of emerging ultrasound techniques and algorithms for the management of small HCC"
| Modalities | Function | Advantages | Limitations |
| US, ultrasound; LI-RADS, Liver Imaging Reporting and Data System; HCC, hepatocellular carcinoma; CEUS, contrast-enhanced ultrasound; CT, computed tomography; MRI, magnetic resonance imaging; APHE, arterial phase hyperenhancement; TRA, treatment response assessment. | |||
| B-mode US | To detect and characterize lesion as well as to assess adjacent invasion | First-line tool for screening | Suboptimal sensitivity Suboptimal specificity Influenced by patient, operator and ultrasonic device conditions |
| US LI-RADS | To standardize B-mode US interpretation, reporting and treatment recommendations in patients at high-risk of HCC | US category score determines follow-up management US visualization score conveys expected sensitivity level of US test Moderate-to-good intra-observer agreement | Lack of management recommendations based on visualization scores Confounding factors: overweight, Child-Pugh class B disease, and moderate to severe fatty liver |
| Traditional Doppler US | To visualize the nature, direction and velocity of blood flow as well as to display its adjacency to intrahepatic vessels | Resistance index aids in differential diagnosis of malignancy | Hard to detect fine blood flow High false negative rate Heartbeat interference |
| Microvascular US | To detect slow-velocity flow and to visualize smaller vessel flow | High vascular sensitivity High spatial resolution Excellent interobserver agreement Reduced motion artifact | Angle dependent Cannot provide directional flow and quantitative evaluation Confounding factors (patient body habitus and motion, deep lesion) |
| CEUS | To observe lesion microperfusion dynamically | The only US technique recommended for HCC diagnosis Detect eHCC that invisible on B-mode US Suitable for CT/MRI contradication No renal toxicity | Few lesions can be characterized at one session Lower sensitivity than CT/MRI Confounding factors (respiration, lesion visualization and operator experience) |
| CEUS LI-RADS | To stratify the likelihood of HCC by imaging appearance on CEUS and lesion size | High interobserver consistency in assessing APHE High specificity for CEUS LR-5 The most widely applied CEUS reference for HCC diagnosis | Poor to moderate interobserver consistency in assessing washout CEUS LR-3 reduces the HCC diagnostic probability Poor sensitivity for CEUS LR-5 Current version not available for Sonazoid contrast agent |
| Super resolution US | To precisely localize and track microbubble for ultrahigh-resolution vascular imaging | 10 times better spatial resolution than CEUS Wide flow velocity measurement range mm/s to cm/s and independent of Doppler angle | Slow imaging speeds Susceptibility to probe or tissue motion Fails to resolve the complete capillary bed |
| US elastography | To detect tissue stiffness by measuring the elasticity coefficient | Good reproducibility with same device Accuracy for liver fibrosis staging High liver stiffness is related to HCC occurrence | Overlap of stiffness value for benign and malignant lesions Confounding factors (sampling bias, lesion depth, necroinflammation, congestion, manufacture) |
| US radiomics | To extract imaging features from US images in a high throughput manner | Detect information unrecognizable to naked eye Avoid interpretation subjectivity | Poor interpretability and generalization Input data may vary from different device and operators Lack of standardization |
| Intraoperative US | To provide high-resolution imaging by directly placing transducer on liver surface | High sensitivity in detecting small lesions High spatial resolution High diagnostic accuracy Unaffected by gas, ribs and other structures Immediate imaging and interpretation | Operators need to be experienced Some lesions remain difficult to visualize Difficult to show the whole liver |
| US fusion imaging | To fuse and reconstruct US/CEUS image with previous cross-sectional images in real time | Detect invisible lesions on B-mode US or CEUS High positioning accuracy High technical success rate Low complication rate | Operation complexity Operator dependent Not suitable for patient with anatomical abnormality |
| LI-RADS CEUS nonradiation TRA v2024 | To provide instructions for tumor viability evaluation after non-radiation locoregional therapy | Evaluation based on both intralesional and perilesional contrast enhancement Broader criteria for intralesional enhancement and stricter criteria are used for perilesional enhancement | LR-TR Nonviable does not imply complete pathologic response Indications only include partial locoregional treatment Limited current studies |
| [1] |
Chan SL , Sun HC , Xu Y , Zeng H , El-Serag HB , Lee JM , et al . The Lancet Commission on addressing the global hepatocellular carcinoma burden: comprehensive strategies from prevention to treatment. Lancet 2025; 406: 731-778.
doi: 10.1016/S0140-6736(25)01042-6 |
| [2] |
Singal AG , Lampertico P , Nahon P . Epidemiology and surveillance for hepatocellular carcinoma: new trends. J Hepatol 2020; 72: 250-261.
doi: 10.1016/j.jhep.2019.08.025 |
| [3] |
Reig M , Forner A , Rimola J , Ferrer-Fabrega J , Burrel M , Garcia-Criado A , et al . BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol 2022; 76: 681-693.
doi: 10.1016/j.jhep.2021.11.018 |
| [4] |
European Association for the Study of the Liver . EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2018; 69: 182-236.
doi: 10.1016/j.jhep.2018.03.019 |
| [5] |
Marrero JA , Kulik LM , Sirlin CB , Zhu AX , Finn RS , Abecassis MM , et al . Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 2018; 68: 723-750.
doi: 10.1002/hep.29913 |
| [6] |
Xie DY , Zhu K , Ren ZG , Zhou J , Fan J , Gao Q . A review of 2022 Chinese clinical guidelines on the management of hepatocellular carcinoma: updates and insights. Hepatobiliary Surg Nutr 2023; 12: 216-228.
doi: 10.21037/hbsn-22-469 |
| [7] |
Omata M , Cheng AL , Kokudo N , Kudo M , Lee JM , Jia J , et al . Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int 2017; 11: 317-370.
doi: 10.1007/s12072-017-9799-9 |
| [8] |
Faccia M , Garcovich M , Ainora ME , Riccardi L , Pompili M , Gasbarrini A , et al . Contrast-enhanced ultrasound for monitoring treatment response in different stages of hepatocellular carcinoma. Cancers (Basel) 2022; 14: 481.
doi: 10.3390/cancers14030481 |
| [9] |
Yang D , Chen X , Huang L , Wang X , Mao L , Lin L , et al . Correlation between CEUS LI-RADS categorization of HCC < 20 mm and clinic-pathological features. Insights Imaging 2024; 15: 110.
doi: 10.1186/s13244-024-01688-7 |
| [10] |
Fan PL , Ding H , Mao F , Chen LL , Dong Y , Wang WP . Enhancement patterns of small hepatocellular carcinoma (</= 30 mm) on contrast-enhanced ultrasound: correlation with clinicopathologic characteristics. Eur J Radiol 2020; 132: 109341.
doi: 10.1016/j.ejrad.2020.109341 |
| [11] |
European Association for the Study of the Liver . EASL Clinical Practice Guidelines on the management of hepatocellular carcinoma. J Hepatol 2025; 82: 315-374.
doi: 10.1016/j.jhep.2024.08.028 |
| [12] | Korean Liver Cancer Association, 2022 KLCA-NCC Korea Practice Guidelines for the management of hepatocellular carcinoma. Korean J Radiol 2022; 23:1126-1240. |
| [13] |
Kudo M , Kawamura Y , Hasegawa K , Tateishi R , Kariyama K , Shiina S , et al . Management of hepatocellular carcinoma in Japan: JSH consensus statements and recommendations 2021 update. Liver Cancer 2021; 10: 181-223.
doi: 10.1159/000514174 |
| [14] |
Desjonqueres E , Campani C , Marra F , Zucman-Rossi J , Nault JC . Preneoplastic lesions in the liver: molecular insights and relevance for clinical practice. Liver Int 2022; 42: 492-506.
doi: 10.1111/liv.15152 |
| [15] |
International Consensus Group for Hepatocellular Neoplasia . Pathologic diagnosis of early hepatocellular carcinoma: a report of the international consensus group for hepatocellular neoplasia. Hepatology 2009; 49: 658-664.
doi: 10.1002/hep.22709 |
| [16] |
Kudo M . Early hepatocellular carcinoma: definition and diagnosis. Liver Cancer 2013; 2: 69-72.
doi: 10.1159/000343842 |
| [17] |
Yang F , Zhao J , Liu C , Mao Y , Mu J , Wei X , et al . Superb microvascular imaging technique in depicting vascularity in focal liver lesions: more hypervascular supply patterns were depicted in hepatocellular carcinoma. Cancer Imaging 2019; 19: 92.
doi: 10.1186/s40644-019-0277-6 |
| [18] |
Singal AG , Zhang E , Narasimman M , Rich NE , Waljee AK , Hoshida Y , et al . HCC surveillance improves early detection, curative treatment receipt, and survival in patients with cirrhosis: a meta-analysis. J Hepatol 2022; 77: 128-139.
doi: 10.1016/j.jhep.2022.01.023 |
| [19] |
Singal A , Volk ML , Waljee A , Salgia R , Higgins P , Rogers MA , et al . Meta-analysis: surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis. Aliment Pharmacol Ther 2009; 30: 37-47.
doi: 10.1111/j.1365-2036.2009.04014.x |
| [20] | Tzartzeva K , Obi J , Rich NE , Parikh ND , Marrero JA , Yopp A , et al. Surveillance imaging and alpha fetoprotein for early detection of hepatocellular carcinoma in patients with cirrhosis: a meta-analysis. Gastroenterology 2018; 154:1706-1718 e1701. |
| [21] |
Son JH , Choi SH , Kim SY , Jang HY , Byun JH , Won HJ , et al . Validation of US Liver Imaging Reporting and Data System version 2017 in patients at high risk for hepatocellular carcinoma. Radiology 2019; 292: 390-397.
doi: 10.1148/radiol.2019190035 |
| [22] |
Park MK , Lee DH , Hur BY , Lee HC , Lee YB , Yu SJ , et al . Effectiveness of US surveillance of hepatocellular carcinoma in chronic hepatitis B: US LI-RADS visualization score. Radiology 2023; 307: e222106.
doi: 10.1148/radiol.222106 |
| [23] |
Bae JS , Lee JM , Jeon SK , Jang S . Comparison of microFlow imaging with color and power Doppler imaging for detecting and characterizing blood flow signals in hepatocellular carcinoma. Ultrasonography 2020; 39: 85-93.
doi: 10.14366/usg.19033 |
| [24] |
Dong Y , Wang WP , Ignee A , Zuo D , Qiu YJ , Zhang Q , et al . The diagnostic value of Doppler resistive index in the differential diagnosis of focal liver lesions. J Ultrason 2023; 23: e45-e52.
doi: 10.15557/JoU.2023.0010 |
| [25] |
Kumada T , Nakano S , Toyoda H , Hayashi K , Kiriyama S , Sone Y , et al . Assessment of tumor hemodynamics in small hepatocellular carcinoma: comparison of Doppler ultrasonography, angiography-assisted computed tomography, and pathological findings. Liver Int 2004; 24: 425-431.
doi: 10.1111/j.1478-3231.2004.0932.x |
| [26] |
Dubinsky TJ , Revels J , Wang S , Toia G , Sonneborn R , Hippe DS , et al . Comparison of superb microvascular imaging with color flow and power Doppler imaging of small hepatocellular carcinomas. J Ultrasound Med 2018; 37: 2915-2924.
doi: 10.1002/jum.14654 |
| [27] |
Cannella R , Pilato G , Mazzola M , Bartolotta TV . New microvascular ultrasound techniques: abdominal applications. Radiol Med 2023; 128: 1023-1034.
doi: 10.1007/s11547-023-01679-6 |
| [28] |
Han H , Ji Z , Huang B , Mao L , Cao Q , Fan P , et al . The preliminary application of simultaneous display of contrast-enhanced ultrasound and micro-flow imaging technology in the diagnosis of hepatic tumors. J Ultrasound Med 2023; 42: 729-737.
doi: 10.1002/jum.16111 |
| [29] |
Jeon SK , Lee JY , Han JK . Superb microvascular imaging technology of ultrasound examinations for the evaluation of tumor vascularity in hepatic hemangiomas. Ultrasonography. 2021; 40: 538-545.
doi: 10.14366/usg.20177 |
| [30] |
Xu HX , Xie XY , Lu MD , Liu GJ , Xu ZF , Zheng YL , et al . Contrast-enhanced sonography in the diagnosis of small hepatocellular carcinoma < or = 2 cm. J Clin Ultrasound 2008; 36: 257-266.
doi: 10.1002/jcu.20433 |
| [31] |
Zhang Z , Ma C , Luo Y . Diagnostic value of liver contrast-enhanced ultrasound in early hepatocellular carcinoma: a systematic review and meta-analysis. J Gastrointest Oncol 2023; 14: 626-635.
doi: 10.21037/jgo-23-211 |
| [32] |
Duisyenbi Z , Numata K , Nihonmatsu H , Fukuda H , Chuma M , Kondo M , et al . Comparison between low mechanical index and high mechanical index contrast modes of contrast-enhanced ultrasonography: evaluation of perfusion defects of hypervascular hepatocellular carcinomas during the post-vascular phase. J Ultrasound Med 2019; 38: 2329-2338.
doi: 10.1002/jum.14926 |
| [33] |
Iavarone M , Sangiovanni A , Forzenigo LV , Massironi S , Fraquelli M , Aghemo A , et al . Diagnosis of hepatocellular carcinoma in cirrhosis by dynamic contrast imaging: the importance of tumor cell differentiation. Hepatology 2010; 52: 1723-1730.
doi: 10.1002/hep.23903 |
| [34] |
Forner A , Vilana R , Bianchi L , Rodriguez-Lope C , Reig M , Garcia-Criado MA , et al . Lack of arterial hypervascularity at contrast-enhanced ultrasound should not define the priority for diagnostic work-up of nodules < 2 cm. J Hepatol 2015; 62: 150-155.
doi: 10.1016/j.jhep.2014.08.028 |
| [35] |
Kudo M , Ueshima K , Osaki Y , Hirooka M , Imai Y , Aso K , et al . B-Mode ultrasonography versus contrast-enhanced ultrasonography for surveillance of hepatocellular carcinoma: a prospective multicenter randomized controlled trial. Liver Cancer 2019; 8: 271-280.
doi: 10.1159/000501082 |
| [36] | Ren J , Lu Q , Fei X , Dong Y , D Onofrio M , Sidhu PS , et al . Assessment of arterial-phase hyperenhancement and late-phase washout of hepatocellular carcinoma-a meta-analysis of contrast-enhanced ultrasound (CEUS) with SonoVue(R) and Sonazoid(R). Eur Radiol 2024; 34: 3795-3812 |
| [37] |
Goto E , Masuzaki R , Tateishi R , Kondo Y , Imamura J , Goto T , et al . Value of post-vascular phase (Kupffer imaging) by contrast-enhanced ultrasonography using Sonazoid in the detection of hepatocellular carcinoma. J Gastroenterol 2012; 47: 477-485.
doi: 10.1007/s00535-011-0512-9 |
| [38] |
Sugimoto K , Moriyasu F , Saito K , Taira J , Saguchi T , Yoshimura N , et al . Comparison of Kupffer-phase Sonazoid-enhanced sonography and hepatobiliary-phase gadoxetic acid-enhanced magnetic resonance imaging of hepatocellular carcinoma and correlation with histologic grading. J Ultrasound Med 2012; 31: 529-538.
doi: 10.7863/jum.2012.31.4.529 |
| [39] |
Ling W , Wang M , Ma X , Qiu T , Li J , Lu Q , et al . The preliminary application of liver imaging reporting and data system (LI-RADS) with contrast-enhanced ultrasound (CEUS) on small hepatic nodules (≤ 2 cm). J Cancer 2018; 9: 2946-2952.
doi: 10.7150/jca.25539 |
| [40] |
Huang JY , Li JW , Lu Q , Luo Y , Lin L , Shi YJ , et al . Diagnostic accuracy of CEUS LI-RADS for the characterization of liver nodules 20 mm or smaller in patients at risk for hepatocellular carcinoma. Radiology 2020; 294: 329-339.
doi: 10.1148/radiol.2019191086 |
| [41] |
Zheng W , Li Q , Zou XB , Wang JW , Han F , Li F , et al . Evaluation of contrast-enhanced US LI-RADS version 2017: application on 2020 liver nodules in patients with hepatitis B infection. Radiology 2020; 294: 299-307.
doi: 10.1148/radiol.2019190878 |
| [42] | Wu J , Zhao Q , Wang Y , Xiao F , Cai W , Liu S , et al . Feeding artery: a valuable feature for differentiation of regenerative nodule, dysplastic nodules and small hepatocellular carcinoma in CEUS LI-RADS. Eur Radiol 2024; 34: 745-754 |
| [43] |
Takahashi H , Sugimoto K , Kamiyama N , Sakamaki K , Kakegawa T , Wada T , et al . Noninvasive diagnosis of hepatocellular carcinoma on Sonazoid-enhanced US: value of the kupffer phase. Diagnostics (Basel) 2022; 12: 141.
doi: 10.3390/diagnostics12010141 |
| [44] |
Dencks S , Lowerison M , Hansen-Shearer J , Shin Y , Schmitz G , Song P , et al . Super-resolution ultrasound: from data acquisition and motion correction to localization, tracking, and evaluation. IEEE Trans Ultrason Ferroelectr Freq Control 2025; 72: 408-426.
doi: 10.1109/TUFFC.2025.3543322 |
| [45] |
Hingot V , Errico C , Heiles B , Rahal L , Tanter M , Couture O . Microvascular flow dictates the compromise between spatial resolution and acquisition time in ultrasound localization microscopy. Sci Rep 2019; 9: 2456.
doi: 10.1038/s41598-018-38349-x |
| [46] |
Zeng QQ , An SZ , Chen CN , Wang Z , Liu JC , Wan MX , et al . Focal liver lesions: multiparametric microvasculature characterization via super-resolution ultrasound imaging. Eur Radiol Exp 2024; 8: 138.
doi: 10.1186/s41747-024-00540-3 |
| [47] |
Wang F , Yu J , Lu X , Numata K , Ruan L , Zhang D , et al . Relationship between contrast-enhanced ultrasound combined with ultrasound resolution microscopy imaging and histological features of hepatocellular carcinoma. Abdom Radiol (NY) 2025; 50: 3530-3542.
doi: 10.1007/s00261-025-04825-y |
| [48] |
Jin YJ , Kim HY , Suh YJ , Lee CH , Yu JH , Kim MN , et al . Risk assessment of hepatitis B virus-related hepatocellular carcinoma development using vibration-controlled transient elastography: systematic review and meta-analysis. Clin Mol Hepatol 2024; 30: S159-S171.
doi: 10.3350/cmh.2024.0163 |
| [49] |
Li JW , Ling WW , Lu Q , Lu CL , He D , Luo Y . Liver stiffness and serum alpha-fetoprotein in discriminating small hepatocellular carcinoma from cirrhotic nodule. Ultrasound Q 2016; 32: 319-326.
doi: 10.1097/RUQ.0000000000000244 |
| [50] |
Jiang D , Qian Y , Gu YJ , Wang R , Yu H , Dong H , et al . Predicting hepatocellular carcinoma: a new non-invasive model based on shear wave elastography. World J Gastroenterol 2024; 30: 3166-3178.
doi: 10.3748/wjg.v30.i25.3166 |
| [51] |
Pierce TT , Ozturk A , Sherlock SP , Moura Cunha G , Wang X , Li Q , et al . Reproducibility and repeatability of US shear-wave and transient elastography in nonalcoholic fatty liver disease. Radiology 2024; 312: e233094.
doi: 10.1148/radiol.233094 |
| [52] |
Yang Q , Wei J , Hao X , Kong D , Yu X , Jiang T , et al . Improving B-mode ultrasound diagnostic performance for focal liver lesions using deep learning: a multicentre study. EBioMedicine 2020; 56: 102777.
doi: 10.1016/j.ebiom.2020.102777 |
| [53] |
Lu RF , She CY , He DN , Cheng MQ , Wang Y , Huang H , et al . AI enhanced diagnostic accuracy and workload reduction in hepatocellular carcinoma screening. NPJ Digit Med 2025; 8: 500.
doi: 10.1038/s41746-025-01892-9 |
| [54] |
Du Z , Fan F , Ma J , Liu J , Yan X , Chen X , et al . Development and validation of an ultrasound-based interpretable machine learning model for the classification of ≤ 3 cm hepatocellular carcinoma: a multicentre retrospective diagnostic study. EClinicalMedicine 2025; 81: 103098.
doi: 10.1016/j.eclinm.2025.103098 |
| [55] |
Ding W , Meng Y , Ma J , Pang C , Wu J , Tian J , et al . Contrast-enhanced ultrasound-based AI model for multi-classification of focal liver lesions. J Hepatol 2025; 83: 426-439.
doi: 10.1016/j.jhep.2025.01.011 |
| [56] |
Xian MF , Lan WT , Zhang Z , Li MD , Lin XX , Huang Y , et al . Enhancing hepatocellular carcinoma diagnosis in non-high-risk patients: a customized ChatGPT model integrating contrast-enhanced ultrasound. Radiol Med 2025; 130: 1013-1023.
doi: 10.1007/s11547-025-01994-0 |
| [57] |
Liu F , Liu D , Wang K , Xie X , Su L , Kuang M , et al . Deep learning radiomics based on contrast-enhanced ultrasound might optimize curative treatments for very-early or early-stage hepatocellular carcinoma patients. Liver Cancer 2020; 9: 397-413.
doi: 10.1159/000505694 |
| [58] |
Wagnetz U , Atri M , Massey C , Wei AC , Metser U . Intraoperative ultrasound of the liver in primary and secondary hepatic malignancies: comparison with preoperative 1.5-T MRI and 64-MDCT. AJR Am J Roentgenol 2011; 196: 562-568.
doi: 10.2214/AJR.10.4729 |
| [59] |
Takigawa Y , Sugawara Y , Yamamoto J , Shimada K , Yamasaki S , Kosuge T , et al . New lesions detected by intraoperative ultrasound during liver resection for hepatocellular carcinoma. Ultrasound Med Biol 2001; 27: 151-156.
doi: 10.1016/S0301-5629(00)00346-X |
| [60] |
Ahn JH , Eom DW , Ryu DS , Park MS , Jung SM , Choi KM , et al . Synchronous multicentric small hepatocellular carcinomas: defining the capsule on high-frequency intraoperative ultrasonography with pathologic correlation. Ultrasonography 2016; 35: 335-344.
doi: 10.14366/usg.16001 |
| [61] |
Iancu I , Bartos A , Cioltean C , Branzila S , Bocse H , Herdean A , et al . Up to date and perspectives for hepatocellular carcinoma\'s intraoperative ultrasound. Chirurgia (Bucur) 2021; 116: 399-408.
doi: 10.21614/chirurgia.116.4.399 |
| [62] |
Wu W , Jing X , Xue GQ , Zhu XL , Wang J , Du RQ , et al . A multicenter randomized controlled study of contrast-enhanced US versus US-guided biopsy of focal liver lesions. Radiology 2022; 305: 721-728.
doi: 10.1148/radiol.212317 |
| [63] |
Peloso A , Franchi E , Canepa MC , Barbieri L , Briani L , Ferrario J , et al . Combined use of intraoperative ultrasound and indocyanine green fluorescence imaging to detect liver metastases from colorectal cancer. HPB (Oxford) 2013; 15: 928-934.
doi: 10.1111/hpb.12057 |
| [64] |
Omichi K , Inoue Y , Hasegawa K , Sakamoto Y , Okinaga H , Aoki T , et al . Differential diagnosis of liver tumours using intraoperative real-time tissue elastography. Br J Surg 2015; 102: 246-253.
doi: 10.1002/bjs.9728 |
| [65] | da Silva NPB , Hornung M , Beyer LP , Hackl C , Brunner S , Schlitt HJ , et al . Intraoperative shear wave elastography vs. contrast-enhanced ultrasound for the characterization and differentiation of focal liver lesions to optimize liver tumor surgery. Ultraschall Med 2019; 40: 205-211 |
| [66] |
European Society of Radiology . Abdominal applications of ultrasound fusion imaging technique: liver, kidney, and pancreas. Insights Imaging 2019; 10: 6.
doi: 10.1186/s13244-019-0692-z |
| [67] |
Zhou Y , Wang Y , Wang F , Zhang X , Ding J , Zhou H , et al . Additional diagnostic value of fusion imaging of CEUS and first CEUS of invisible hepatic lesions ≤ 2 cm. J Ultrasound Med 2021; 40: 1173-1181.
doi: 10.1002/jum.15498 |
| [68] |
Calandri M , Mauri G , Yevich S , Gazzera C , Basile D , Gatti M , et al . Fusion imaging and virtual navigation to guide percutaneous thermal ablation of hepatocellular carcinoma: a review of the literature. Cardiovasc Intervent Radiol 2019; 42: 639-647.
doi: 10.1007/s00270-019-02167-z |
| [69] | Huang Q , Zeng Q , Long Y , Tan L , Zheng R , Xu E , et al . Fusion imaging techniques and contrast-enhanced ultrasound for thermal ablation of hepatocellular carcinoma - a prospective randomized controlled trial. Int J Hyperthermia 2019; 36: 1207-1215 |
| [70] |
Melendez-Torres J , Singal AG . Early detection of hepatocellular carcinoma: roadmap for improvement. Expert Rev Anticancer Ther 2022; 22: 621-632.
doi: 10.1080/14737140.2022.2074404 |
| [71] |
Huang H , Cheng MQ , He DN , Xian MF , Zeng D , Wu SH , et al . US LI-RADS in surveillance for recurrent hepatocellular carcinoma after curative treatment. Eur Radiol 2023; 33: 9357-9367.
doi: 10.1007/s00330-023-09903-7 |
| [72] |
Hong SK , Jin XL , Suh S , Hong SY , Hong K , Han ES , et al . Different risk factors for early and late recurrence after curative resection of hepatocellular carcinoma. World J Surg 2022; 46: 197-206.
doi: 10.1007/s00268-021-06308-9 |
| [73] |
Hai Y , Savsani E , Chong W , Eisenbrey J , Lyshchik A . Meta-analysis and systematic review of contrast-enhanced ultrasound in evaluating the treatment response after locoregional therapy of hepatocellular carcinoma. Abdom Radiol (NY) 2021; 46: 5162-5179.
doi: 10.1007/s00261-021-03248-9 |
| [74] |
Lyshchik A , Fetzer DT , Kono Y , Wilson SR , Dietrich CF , Clevert DA , et al . Liver Imaging Reporting and Data System Contrast-Enhanced US Nonradiation Treatment Response Assessment version 2024. Radiology 2024; 311: e232369.
doi: 10.1148/radiol.232369 |
| [75] |
Deng H , Shang W , Wang K , Guo K , Liu Y , Tian J , et al . Targeted-detection and sequential-treatment of small hepatocellular carcinoma in the complex liver environment by GPC-3-targeted nanoparticles. J Nanobiotechnology 2022; 20: 156.
doi: 10.1186/s12951-022-01378-w |
| [76] | Qi S , Liu G , Chen J , Cao P , Lei X , Ding C , et al . Targeted multifunctional nanoplatform for imaging-guided precision diagnosis and photothermal/photodynamic therapy of orthotopic hepatocellular carcinoma. Int J Nanomedicine 2022; 17: 3777-3792 |
| [77] |
Baron Toaldo M , Salvatore V , Marinelli S , Palama C , Milazzo M , Croci L , et al . Use of VEGFR-2 targeted ultrasound contrast agent for the early evaluation of response to sorafenib in a mouse model of hepatocellular carcinoma. Mol Imaging Biol 2015; 17: 29-37.
doi: 10.1007/s11307-014-0764-x |
| [78] |
Zhang C , Zhang Q , Xu Q , Jiang X , Ma Y , Liu C , et al . Ultrasound targeted microbubbles for theranostic applications in liver diseases: from molecular imaging to targeted therapy. Drug Deliv 2025; 32: 2541656.
doi: 10.1080/10717544.2025.2541656 |
| [1] | Li Yanran, Cui Yuanjie, Wu Qingqing, Zhang Na. Current Applications of Artificial Intelligence in Obstetric Ultrasound [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 449-456. |
| [2] | Hou Wenfei, Chen Wanting, Liu Huazhen, Tang Jiajia, Yang Meng. Applications of Ultrasound Localization Microscopy in Abdominal Imaging [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 347-356. |
| [3] | Yu Xiao jie, Song Zheng lai, Chang Xue yong, Yu Jie, Liang Ping. Artificial Intelligence in Ultrasound Diagnosis of Liver Nodules: A Comprehensive Review of B-Mode and Contrast-enhanced Applications [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 326-346. |
| [4] | Zhong Xian, Xie Xiaoyan. Multimodal Ultrasound Radiomics in Liver Disease: Current Status and Future Directions [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 388-408. |
| [5] | Zhang Xiaoqian, Zhang Jingwen, Dong Yijie, Zhou Jianqiao. Research Progress and Clinical Translation of Photoacoustic–ultrasound Fusion Imaging in Breast Cancer Diagnosis and Therapy [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 467-482. |
| [6] | Jin Tong, Yu Xiaohu, Ai Zheng, Guo Hongcheng. Artificial Intelligence in Ultrasound Imaging: A Review of Progress from Machine Learning to Large Language Model [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 483-496. |
| [7] | Xiang Xi, Yang Yujia, Wang Liyun, Qiu Li. Advances and Applications in Dermatological Ultrasound [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 457-466. |
| [8] | Zheng Hairong, Meng Long, Li Fei, Niu Lili, Qiu Weibao, Ma Teng, Liu Chengbo, Zhu Xuefeng, Wan Liwen, Cai Feiyan. Advance in Ultrasound Super-resolution Imaging, Cell Manipulation and Inter-brain Communication [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(4): 307-325. |
| [9] | Yang Jie, Liu Xiaodi, Wang Wenhui, Liao Min, Wu Zhe, Galeano July, Perez-Buitrago Sandra, Lu Qiang. Therapeutic Focused Ultrasound: Advances in Antitumor Immunotherapy of Solid Tumors [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(3): 245-253. |
| [10] | Shi Junni, Xu Jiatong, Chen Chuanjian, Xiang Guanghua, Zheng Wen, Chen Man. Ultrasound Viscoelasticity for Breast Tumor: High Diagnostic Performance at the Peritumoral Boundary [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(3): 270-276. |
| [11] | Farooq Syed Muhammad Yousaf, Rasool Kinza, Gilani Syed Amir, Fatima Mehreen, Malik Sajid Shaheen. Inter and Intra-Rater Reliability of Musculoskeletal Ultrasound to Measure Plantar Fascia Thickness in Patients with Established Plantar Fasciitis [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(3): 283-289. |
| [12] | Xia ShuJun, Zheng YuHang, Hua Qing, Wei MinYan, Wen Jing, Luo XiaoMao, Yan JiPing, Bai BaoYan, Liu Fang, Dong YiJie, Zhou JianQiao, behalf of The Chinese Artificial Intelligence Alliance for Thyroid on, Ultrasound Breast. Super-Resolution Ultrasound-Based Habitat Imaging: A Consensus Statement [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 97-102. |
| [13] | Ye Beibei, Zhang Yifeng. Preoperative Diagnosis of Thyroid Follicular Tumor [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 127-137. |
| [14] | Zhang Juan, Shen Cuiqin, Du Lianfang, Li Fan. The Application of Ultrasound in the Pre-operative Evaluation of Cervical Cancer [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 163-170. |
| [15] | Liu Jianjun, Zhang Jun, Xue Yafang, Chen Ying, Qiu Mei, Guo Yanli. Ultrasonographic Characteristics and Outcomes of Fetal Umbilical-portal-systemic Venous Shunts: A Single-center Study [J]. Advanced Ultrasound in Diagnosis and Therapy, 2025, 9(2): 181-188. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
Share: WeChat
Copyright ©2018 Advanced Ultrasound in Diagnosis and Therapy
|
 Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
Advanced Ultrasound in Diagnosis and Therapy (AUDT)
is licensed under a Creative Commons Attribution 4.0 International License.
