CONTENTS
Review Article
- Diagnostic Performance of Superb Microvascular Imaging for Breast Masses: A Systematic Review and Meta-analysis
- Zehui Fu, MD, Siqi Wang, MD, Jian Zhang, MD, Yejun Lu, MD, Xiaomin Mo, MD, Ye He, MD, Chong Wang, MD, Hui Chen, MD
- 2022, 6 (3): 95-103. DOI:10.37015/AUDT.2022.210028
- Abstract ( 541 ) HTML ( 42 ) PDF ( 749KB ) ( 758 )
-
Objective: In the present study, we aimed to evaluate the diagnostic performance of superb microvascular imaging (SMI) for breast masses through a meta-analysis.
Methods: PubMed, EMBASE, Cochrane Library, and Web of Science Core Collection databases, as well as the most comprehensive Chinese academic databases in medicine, such as China Biology Medicine Disc, China National Knowledge Infrastructure, and Wanfang Database, were systematically searched. All included studies used histopathological results as the reference standard. To assess the diagnostic performance, we calculated the pooled sensitivity, specificity, positive likelihood ratio (LR+), negative likelihood ratio (LR-), diagnostic odds ratio (DOR), and the area under the curve (AUC). In addition, a subgroup meta-regression analysis was performed to investigate the heterogeneity.
Results: Fourteen of 1,075 identified articles were included in the current review. The pooled sensitivity, specificity, LR+, LR-, and DOR for SMI were 0.85 (95% CI: 0.79-0.89), 0.80 (95% CI: 0.71-0.87), 4.3 (95% CI: 2.9-6.2), 0.19 (95% CI 0.14-0.26), and 22 (95% CI: 14-36), respectively. The AUC was 0.90 (0.87 - 0.92). Meta-regression showed that there were heterogeneities for sensitivity, but not for specificity.
Conclusions: SMI had good sensitivity, specificity, and excellent diagnostic value in distinguishing benign breast masses from malignant masses and could potentially help select suspicious breast masses for surgery.
Original Research
- Contrast-enhanced Ultrasound for Evaluation of Active Needle Tract Bleeding during Thermal Ablation of Liver Cancer
- Huolin Ye, MD, Qiannan Huang, MD, Qingjing Zeng, MD, Xuqi He, MD, Erjiao Xu, MD, Yinglin Long, MD, Kai Li, MD, Rongqin Zheng, MD
- 2022, 6 (3): 104-111. DOI:10.37015/AUDT.2021.210019
- Abstract ( 522 ) HTML ( 22 ) PDF ( 2296KB ) ( 731 )
-
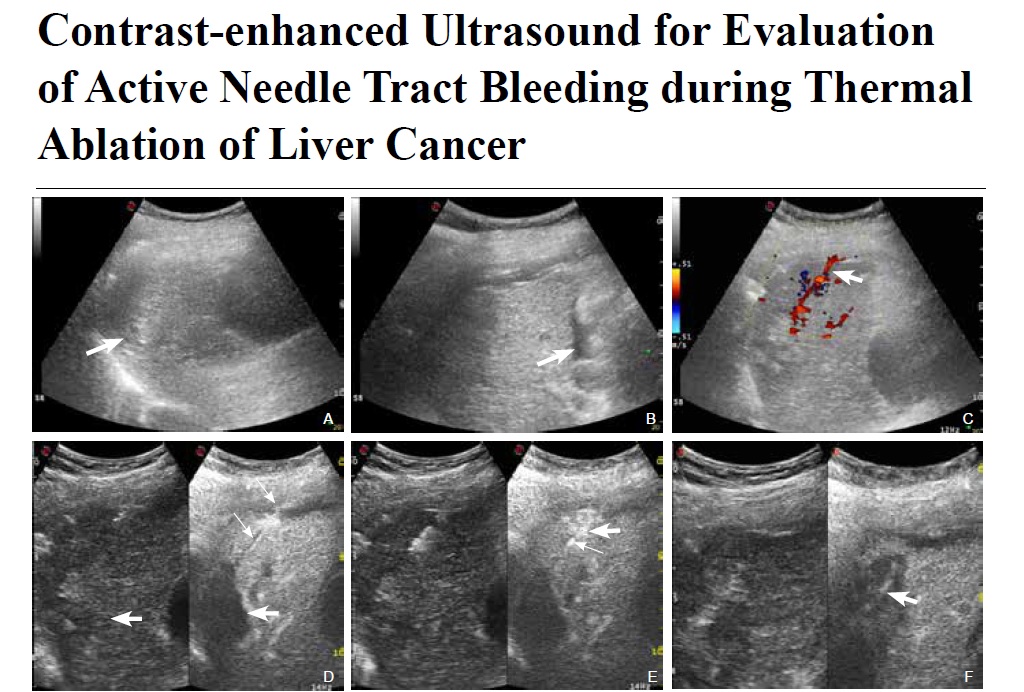
Objective: To investigate the accuracy of contrast-enhanced ultrasound (CEUS) in the diagnosis and localization of active needle-tract bleeding (ANTB) during thermal ablation for liver cancer.
Methods: Between June 2013 and December 2018, liver cancer patients with poor coagulation function or suspected needle-tract bleeding during ablation were enrolled in the study. Conventional US and CEUS were applied to detect ANTB and the bleeding sites, and sequentially abdominal paracentesis drainage (APD) was used as the gold standard for the diagnosis of ANTB. Thermal ablation guided by conventional US or CEUS was used to stop the bleeding.
Results: Among the 77 enrolled patients, 21 patients (27.3%, 21/77) had ANTB. In total, four (19.0%) and 21 (100%) cases of ANTB were diagnosed by colour Doppler US and CEUS, respectively. The sensitivity, specificity and accuracy of colour Doppler US for diagnosing ANTB were 19.0%, 100% and 77.6%, respectively. The sensitivity, specificity, and accuracy of CEUS for diagnosing ANTB were 100%, 100% and 100%, respectively. The sensitivity of CEUS to diagnose ANTB was significantly higher than that of colour Doppler US (P < 0.001). All cases of ANTB were arterial bleeding and were stopped by thermal ablation under the guidance of colour Doppler US or CEUS.
Conclusion: Compared to colour Doppler US, CEUS could detect ANTB with significantly higher sensitivity and accurately guide needle-tract ablation during thermal ablation of liver cancer.
- Role of Lung Ultrasound in Diagnosing and Differentiating Transient Tachypnea of Newborn and Respiratory Distress Syndrome in Preterm Neonates
- Srinivasan S, MD, Neeti Aggarwal, MD, Sushma Makhaik, MD, Anupam Jhobta, MD
- 2022, 6 (3): 112-118. DOI:10.37015/AUDT.2022.210034
- Abstract ( 444 ) HTML ( 20 ) PDF ( 851KB ) ( 692 )
-
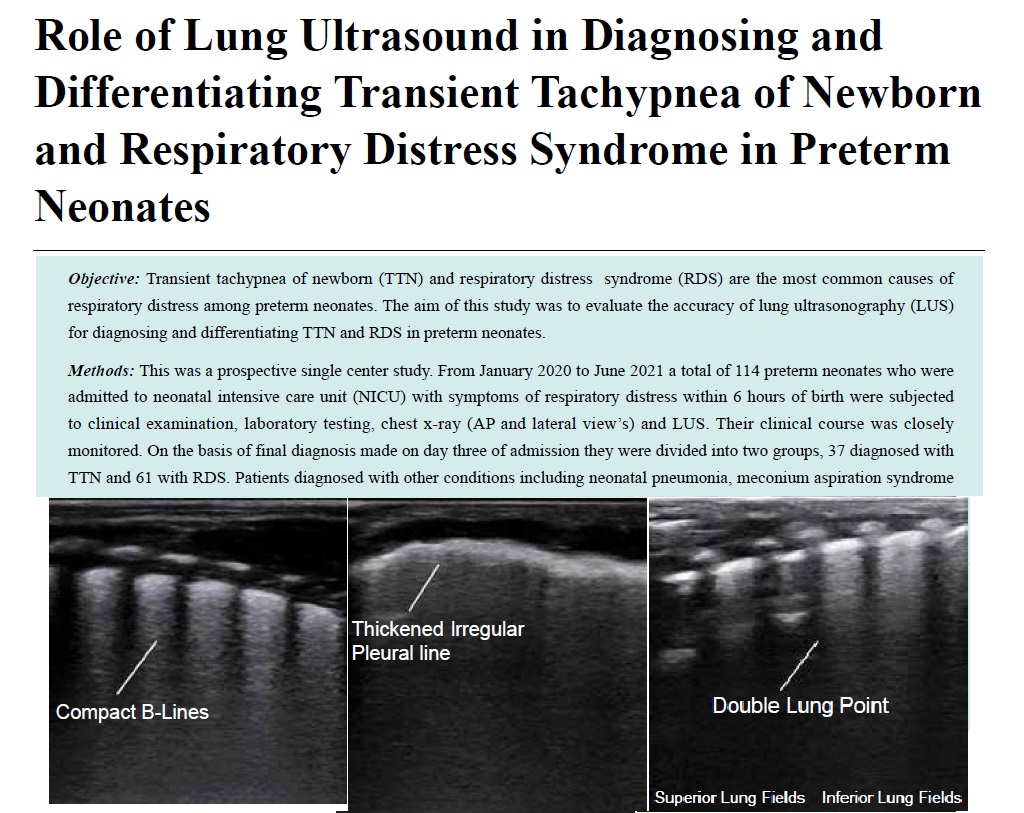
Objective: Transient tachypnea of newborn (TTN) and respiratory distress syndrome (RDS) are the most common causes of respiratory distress among preterm neonates. The aim of this study was to evaluate the accuracy of lung ultrasonography (LUS) for diagnosing and differentiating TTN and RDS in preterm neonates.
Methods: This was a prospective single center study. From January 2020 to June 2021 a total of 114 preterm neonates who were admitted to neonatal intensive care unit (NICU) with symptoms of respiratory distress within 6 hours of birth were subjected to clinical examination, laboratory testing, chest x-ray (AP and lateral view’s) and LUS. Their clinical course was closely monitored. On the basis of final diagnosis made on day three of admission they were divided into two groups, 37 diagnosed with TTN and 61 with RDS. Patients diagnosed with other conditions including neonatal pneumonia, meconium aspiration syndrome etc. were excluded from analysis. LUS findings in RDS and TTN were analyzed and compared to each other.
Results: Pulmonary edema manifesting as alveolo-interstitial syndrome, double lung point and less commonly as white out lungs in absence of consolidation had a 100% sensitivity and specificity in diagnosing TTN. A combination of three signs of consolidation with air or fluid bronchograms, white out lungs and absent spared areas has a 100% sensitivity and specificity for diagnosing RDS. Double lung point was seen only in infants suffering from TTN while consolidation with air or fluid bronchograms was only seen in cases of RDS.
Conclusion: Lung ultrasound can accurately diagnose and reliably differentiate TTN and RDS in preterm neonates. Hence LUS can become an initial screening tool in NICU.
- Ultrasound and Color Doppler Flow Imaging of Paratesticular Leiomyoma
- Nianyu Xue, MM, Yaya Chen, MD, Guoyao Wang, BS, Shengmin Zhang, BS
- 2022, 6 (3): 119-121. DOI:10.37015/AUDT.2021.210022
- Abstract ( 527 ) HTML ( 5 ) PDF ( 836KB ) ( 715 )
-
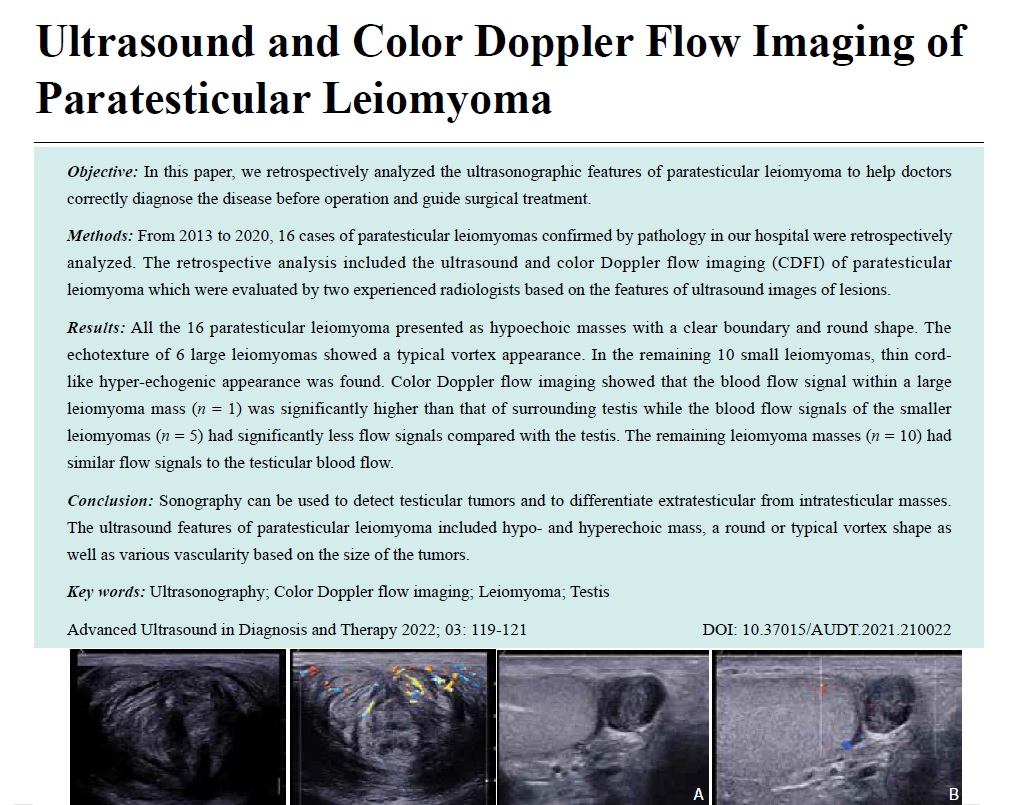
Objective: In this paper, we retrospectively analyzed the ultrasonographic features of paratesticular leiomyoma to help doctors correctly diagnose the disease before operation and guide surgical treatment.
Methods: From 2013 to 2020, 16 cases of paratesticular leiomyomas confirmed by pathology in our hospital were retrospectively analyzed. The retrospective analysis included the ultrasound and color Doppler flow imaging (CDFI) of paratesticular leiomyoma which were evaluated by two experienced radiologists based on the features of ultrasound images of lesions.
Results: All the 16 paratesticular leiomyoma presented as hypoechoic masses with a clear boundary and round shape. The echotexture of 6 large leiomyomas showed a typical vortex appearance. In the remaining 10 small leiomyomas, thin cord-like hyper-echogenic appearance was found. Color Doppler flow imaging showed that the blood flow signal within a large leiomyoma mass (n = 1) was significantly higher than that of surrounding testis while the blood flow signals of the smaller leiomyomas (n = 5) had significantly less flow signals compared with the testis. The remaining leiomyoma masses (n = 10) had similar flow signals to the testicular blood flow.
Conclusion: Sonography can be used to detect testicular tumors and to differentiate extratesticular from intratesticular masses. The ultrasound features of paratesticular leiomyoma included hypo- and hyperechoic mass, a round or typical vortex shape as well as various vascularity based on the size of the tumors.
Case Reports
- Contrast-enhanced Ultrasound Features of Lymphoepithelioma-Like Cholangiocarcinoma with Multiple Metastases: A Case Report
- Guiwu Chen, MS, Wenqin Liu, MS, Zhizhong He, PhD, Xiaomin Liao, MS, Yuhuan Xie, PhD
- 2022, 6 (3): 122-124. DOI:10.37015/AUDT.2021.210027
- Abstract ( 433 ) HTML ( 12 ) PDF ( 1160KB ) ( 694 )
-
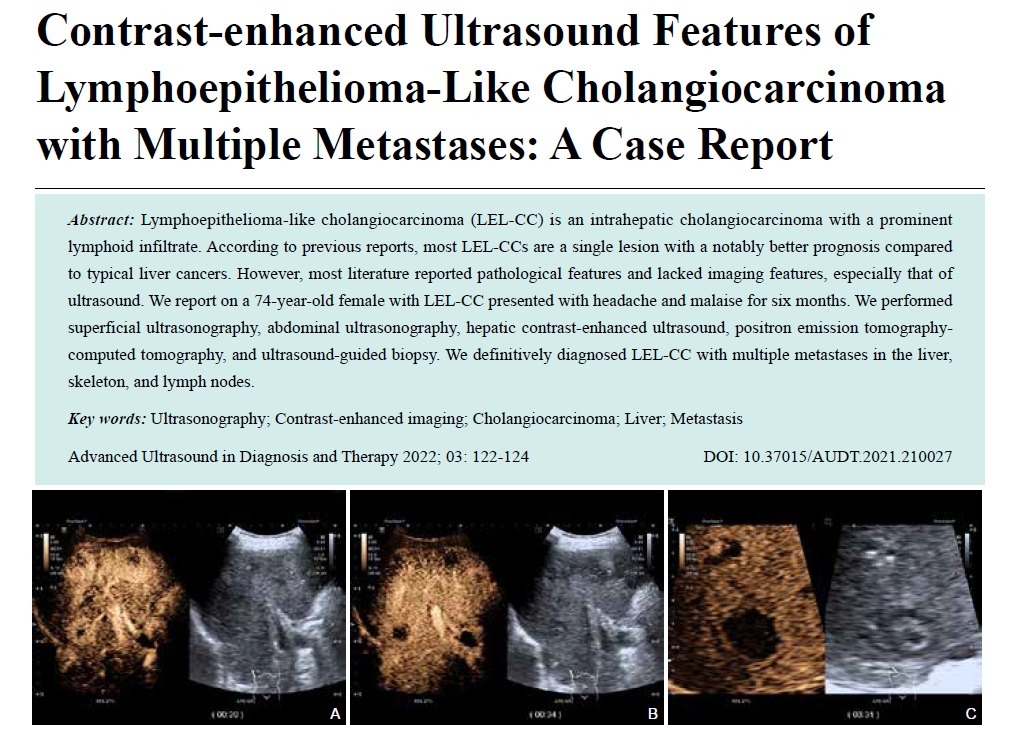
Lymphoepithelioma-like cholangiocarcinoma (LEL-CC) is an intrahepatic cholangiocarcinoma with a prominent lymphoid infiltrate. According to previous reports, most LEL-CCs are a single lesion with a notably better prognosis compared to typical liver cancers. However, most literature reported pathological features and lacked imaging features, especially that of ultrasound. We report on a 74-year-old female with LEL-CC presented with headache and malaise for six months. We performed superficial ultrasonography, abdominal ultrasonography, hepatic contrast-enhanced ultrasound, positron emission tomography-computed tomography, and ultrasound-guided biopsy. We definitively diagnosed LEL-CC with multiple metastases in the liver, skeleton, and lymph nodes.
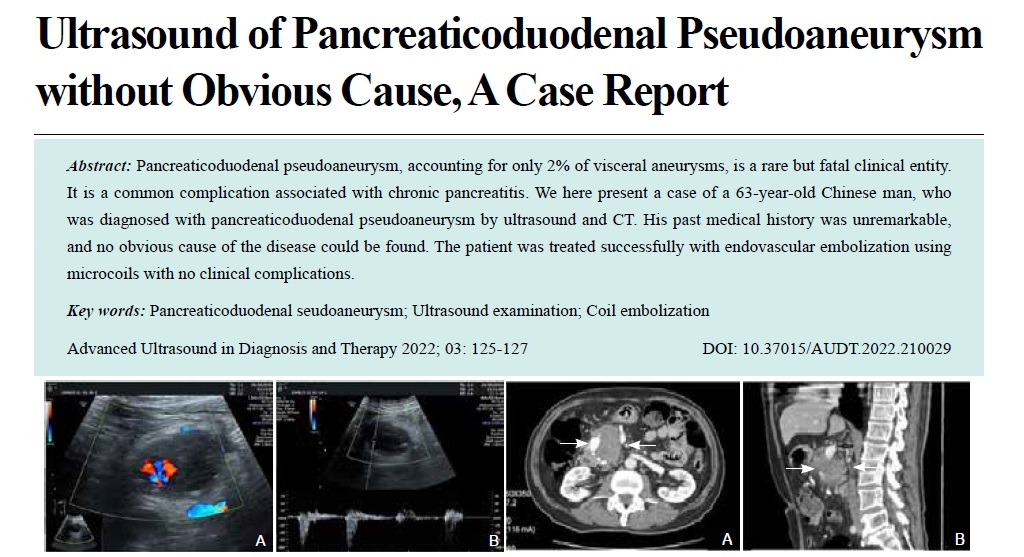
- Ultrasound of Pancreaticoduodenal Pseudoaneurysm without Obvious Cause, A Case Report
- Zi’ang Yang, BS, Xia Xu, BS
- 2022, 6 (3): 125-127. DOI:10.37015/AUDT.2022.210029
- Abstract ( 409 ) HTML ( 12 ) PDF ( 784KB ) ( 687 )
-
Pancreaticoduodenal pseudoaneurysm, accounting for only 2% of visceral aneurysms, is a rare but fatal clinical entity. It is a common complication associated with chronic pancreatitis. We here present a case of a 63-year-old Chinese man, who was diagnosed with pancreaticoduodenal pseudoaneurysm by ultrasound and CT. His past medical history was unremarkable, and no obvious cause of the disease could be found. The patient was treated successfully with endovascular embolization using microcoils with no clinical complications.