Review Article
- CT Perfusion Imaging: A Valuable and Feasible Resolution of Pulmonary Nodules
- Mai-lin Chen, MD, Ying-shi Sun, MD
- 2019, 3 (2): 27-34. DOI:10.37015/AUDT.2019.190806
- Abstract ( 413 ) HTML ( 21 ) PDF ( 3095KB ) ( 744 )
-
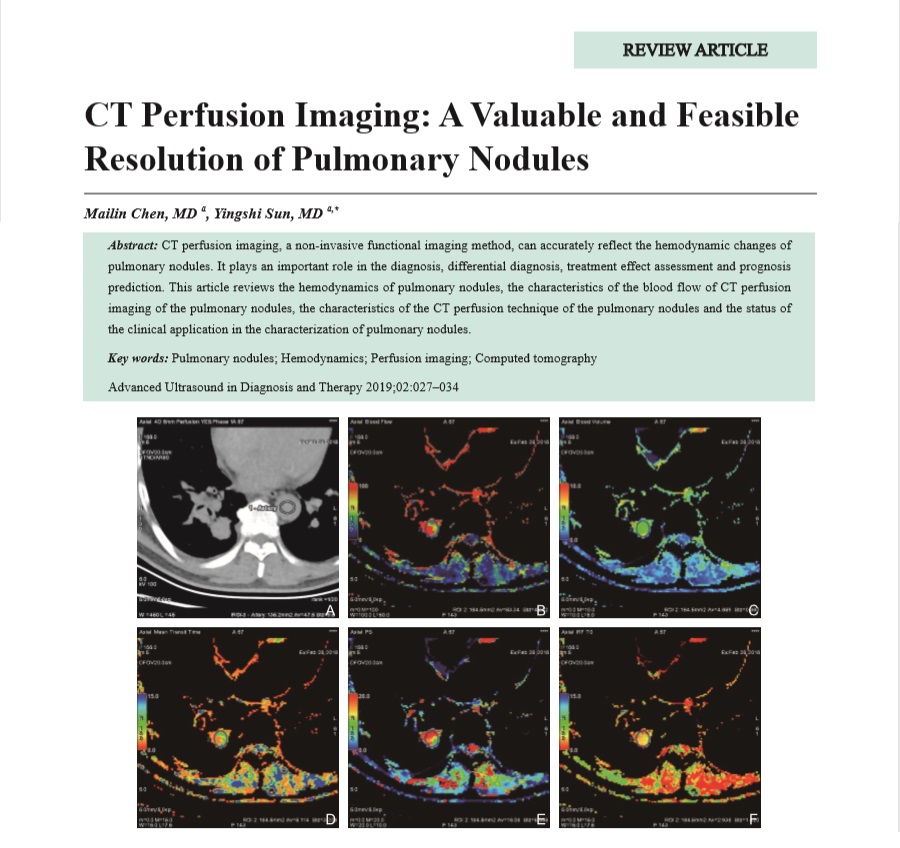
CT perfusion imaging, a non-invasive functional imaging method, can accurately reflect the hemodynamic changes of pulmonary nodules. It plays an important role in the diagnosis, differential diagnosis, treatment effect assessment and prognosis prediction. This article reviews the hemodynamics of pulmonary nodules, the characteristics of the blood flow of CT perfusion imaging of the pulmonary nodules, the characteristics of the CT perfusion technique of the pulmonary nodules and the status of the clinical application in the characterization of pulmonary nodules.
Original Research
- Morphology and Hemodynamic Characteristics of Internal Jugular Vein Hypoplasia and Relation with Cerebral Venous Sinus Stenosis
- Lingyun Jia, MD, Yang Hua, MD, Xunming Ji, MD, Kaiyuan Zhang, MD, Yu Tang, MD
- 2019, 3 (2): 35-40. DOI:10.37015/AUDT.2019.190807
- Abstract ( 462 ) HTML ( 5 ) PDF ( 865KB ) ( 707 )
-
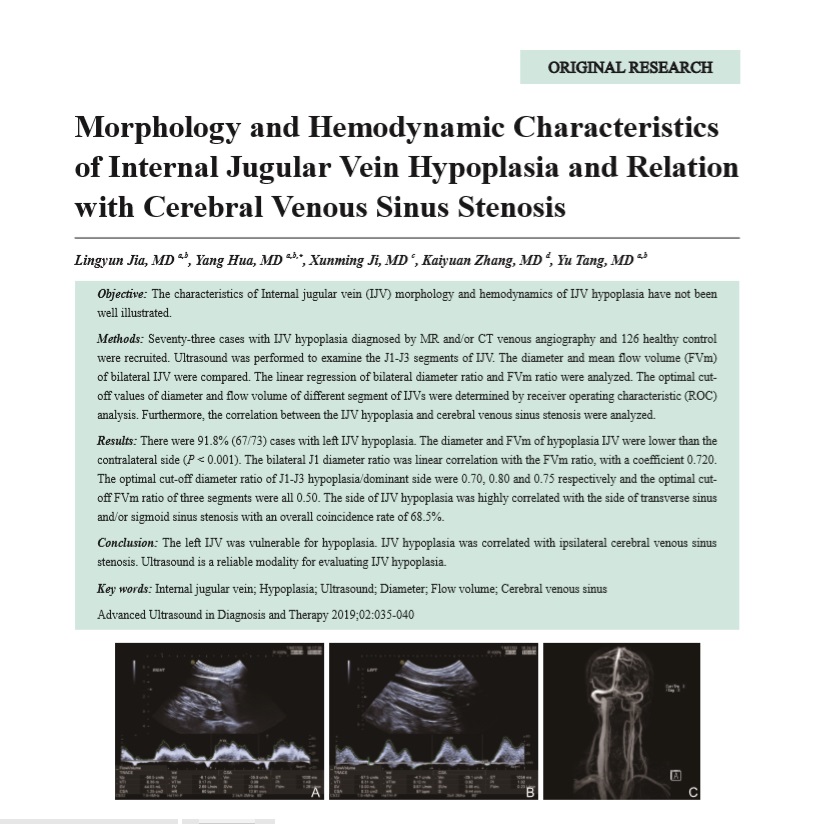
Objective: The characteristics of Internal jugular vein (IJV) morphology and hemodynamics of IJV hypoplasia have not been well illustrated.
Methods: Seventy-three cases with IJV hypoplasia diagnosed by MR and/or CT venous angiography and 126 healthy control were recruited. Ultrasound was performed to examine the J1-J3 segments of IJV. The diameter and mean flow volume (FVm) of bilateral IJV were compared. The linear regression of bilateral diameter ratio and FVm ratio were analyzed. The optimal cutoff values of diameter and flow volume of different segment of IJVs were determined by receiver operating characteristic (ROC) analysis. Furthermore, the correlation between the IJV hypoplasia and cerebral venous sinus stenosis were analyzed.
Results: There were 91.8% (67/73) cases with left IJV hypoplasia. The diameter and FVm of hypoplasia IJV were lower than the contralateral side (P<0.001). The bilateral J1 diameter ratio was linear correlation with the FVm ratio, with a coefficient 0.720. The optimal cut-off diameter ratio of J1-J3 hypoplasia/dominant side were 0.70, 0.80 and 0.75 respectively and the optimal cutoff FVm ratio of three segments were all 0.50. The side of IJV hypoplasia was highly correlated with the side of transverse sinus and/or sigmoid sinus stenosis with an overall coincidence rate of 68.5%.
Conclusion: The left IJV was vulnerable for hypoplasia. IJV hypoplasia was correlated with ipsilateral cerebral venous sinus stenosis. Ultrasound is a reliable modality for evaluating IJV hypoplasia.
- Age-dependent D-dimer Cut-off Value Reduced Unnecessary Ultrasound Scans for Chinese Older Patients Suspected with Deep Vein Thrombosis
- Shunxin Zhang, MD, Cui Liu, MD, Xin Zhao, MD, Danfei Song, MD, Junlai Li, MD
- 2019, 3 (2): 41-46. DOI:10.37015/AUDT.2019.190808
- Abstract ( 428 ) HTML ( 3 ) PDF ( 305KB ) ( 544 )
-
Objective: To evaluate whether the age-dependent D-dimer cut-off value would help to effectively decrease proportion of older patients suspected with deep vein thrombosis (DVT) to take unnecessary ultrasound imaging tests.
Method: This prospective, single institution study was approved by the Institutional Ethics Committee of PLA General Hospital. The patients greater than 65 years with suspected DVT were enrolled in this study and underwent clinical estimations, D-dimer test and ultrasound scans of lower extremity. Clinical probability scores were graded as unlikely (score < 2 and likely (score≥2). Conventional cut-off value (500 μg/L) and age-dependent cut-off value (patient’s age × 10 μg/L) were applied for analyzing respectively. Evaluation and analysis include diagnostic accuracy (sensitivity and specificity), number of false negative results and 95% confidence intervals, and comparison of two cut-off values in different age groups.
Results: A total of 1024 consecutive patients (76.4±19.3 years old) met the inclusion criteria. DVT was present in 256 patients (prevalence 25.0%). In 543 patients (Wells score < 2), DVT could be excluded in 193 patients using conventional cut-off value, while in 277 patients using age-dependent cut-off value, 84 patients could avoid unnecessary ultrasound scans. False negative rates were 3 patients (0.55%, 95% confidence interval 0.11-1.61%) using conventional cut-off vs. 4 patients (0.74%, 95% confidence interval 0.20-1.88%) using age-dependent cut-off value. The absolute increase in patients which DVT could be ruled out using the age-dependent cut-off value was largest in patients > 85 years.
Conclusion: The age-dependent D-dimer cut-off value could help to exclude older patients with suspected DVT, to reduce unnecessary ultrasound scans, and to relieve the financial burden on patients, hospitals and society.
Case Report
- Liver Cancer Microwave Ablation Guided by Imaging Fusion and Needle Tracking Based on Electromagnetic Volume Navigation
- Yupeng Zhu, MD, Wenzhao Liang, MD, Li Ma, MD, Hua Li, MD, Jing Jia, MD, Dezhi Zhang, MD
- 2019, 3 (2): 47-49. DOI:10.37015/AUDT.2019.190809
- Abstract ( 459 ) HTML ( 3 ) PDF ( 1109KB ) ( 605 )
-
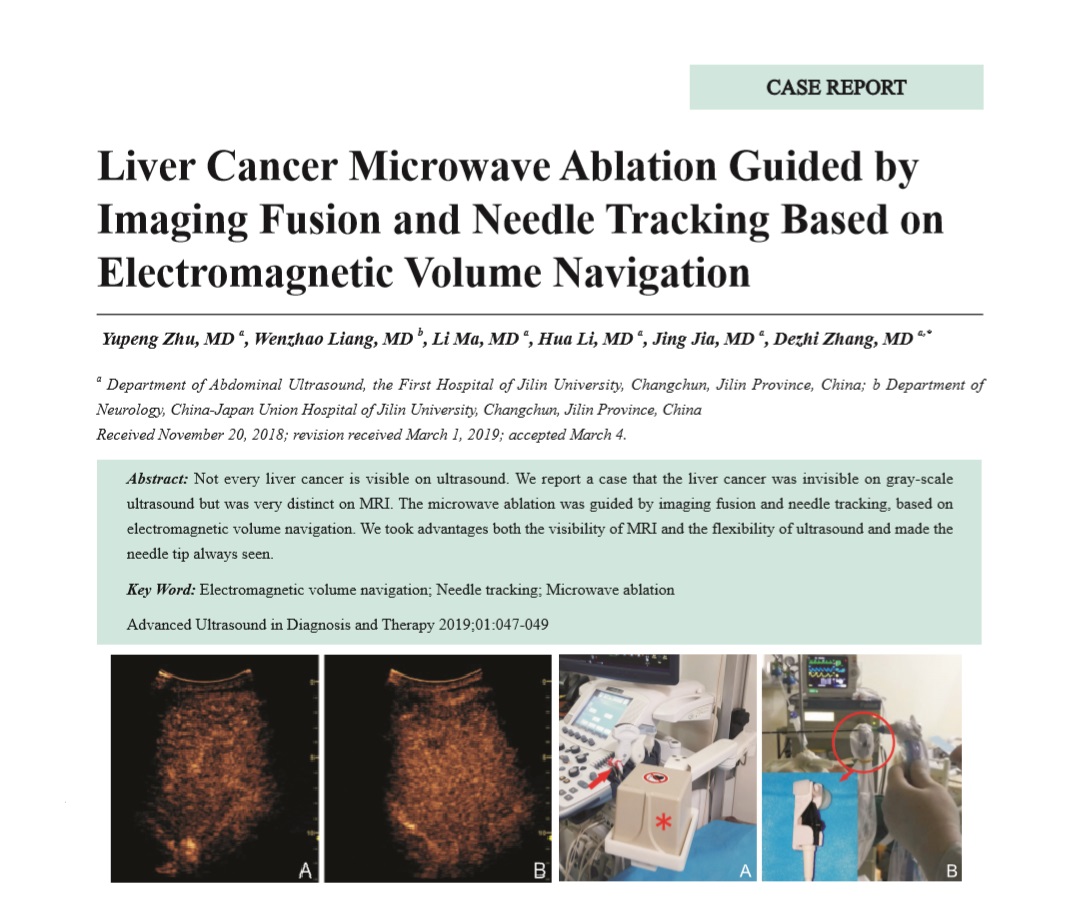
Not every liver cancer is visible on ultrasound. We report a case that the liver cancer was invisible on gray-scale ultrasound but was very distinct on MRI. The microwave ablation was guided by imaging fusion and needle tracking, based on electromagnetic volume navigation. We took advantages both the visibility of MRI and the flexibility of ultrasound and made the needle tip always seen.
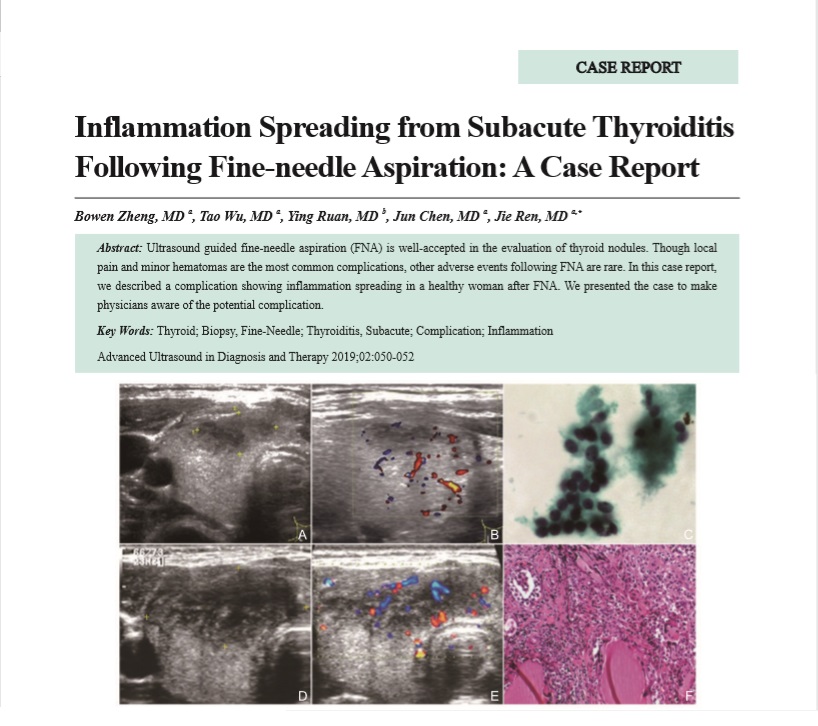
- Inflammation Spreading from Subacute Thyroiditis Following Fine-needle Aspiration: A Case Report
- Bowen Zheng, MD, Tao Wu, MD, Ying Ruan, MD, Jun Chen, MD, Jie Ren, MD
- 2019, 3 (2): 50-52. DOI:10.37015/AUDT.2019.190810
- Abstract ( 388 ) HTML ( 4 ) PDF ( 536KB ) ( 654 )
-
Ultrasound guided fine-needle aspiration (FNA) is well-accepted in the evaluation of thyroid nodules. Though local pain and minor hematomas are the most common complications, other adverse events following FNA are rare. In this case report, we described a complication showing inflammation spreading in a healthy woman after FNA. We presented the case to make physicians aware of the potential complication.